Cannabis, Anxiety, and CBD: Everything You Need to Know
How does cannabis affect you? Do you feel paranoid and anxious after using the herb? Or euphoric and talkative? Cannabis impacts people in different ways. Now, researchers are eyeing up the plant for its role in anxiety. Find out why weed affects people differently, and if it has a place in the future of drug-assisted psychotherapy.
Contents:
- What is anxiety?
- Cannabis for anxiety: an overview
- Thc underpins the cannabis high
- Thc and the biphasic dose response
- Does weed cause or alleviate social anxiety?
- The relationship between cannabidiol and anxiety
- Does cbd produce anxiety?
- Using thc and cbd together
- Terpenes matter
- Timing is important
- Cannabis and psychotherapy: are they compatible?
- Cannabis can help, but shouldn’t be a crutch
- Which cannabis strain to choose?
Does smoking weed cause anxiety? Or does it make the condition worse? It depends on who you ask. Cannabis contains hundreds of interesting phytochemicals. Some of these compounds, including THC and CBD, can interface with receptors that are, incidentally, targets of numerous anti-anxiety medications. Now, researchers are trying to find out if these plant-based molecules can offer beneficial effects through these mechanisms. Find out everything you need to know about cannabis, CBD, and anxiety below.
What Is Anxiety?
Anxiety is an uncontrollable, diffuse, unpleasant, and persistent state of negative affect, characterised by apprehensive anticipation regarding unpredictable and unavoidable future danger, and accompanied by physiological symptoms of tension and a constant state of heightened vigilance. This condition can greatly reduce a person’s quality of life. The condition can occur at any time and ranges from mild to severe. Although it has no single cause, researchers believe both genetic predispositions and environmental factors play a role in its onset.
The most common disease where anxiety is found as the main symptom is generalised anxiety disorder (GAD). This condition affects around 6.8 million[1] adults in the United States alone and can stem alone or from a combination of several factors, including:
| Stress | Past trauma | Genetic inheritance |
| Hormonal imbalance | History of drug abuse | Insomnia |
| Stress | Past trauma | ||||||
| Genetic inheritance | Hormonal imbalance | ||||||
|
History of drug abuse | |||||||
|---|---|---|---|---|---|---|---|
|
Insomnia | |||||||
People diagnosed with GAD often feel restless and worried, have a hard time concentrating, and can even experience dizziness and heart palpitations. GAD can spike during social situations, work, and public gatherings. Ultimately, the condition can rob people of the joy of socialising and enjoying special moments in life. A range of natural lifestyle interventions exist to help tackle the symptoms of GAD, such as:
| Adequate sleep | Meditation | Self-help courses |
| Reducing alcohol and caffeine intake | Regular exercise | Quitting cigarettes |
| Adequate sleep | Meditation |
| Self-help courses | Reducing alcohol and caffeine intake |
| Regular exercise | Quitting cigarettes |
However, these lifestyle changes don’t work for everybody. Some people have to rely on pharmaceuticals to tackle their feelings of anxiety. Yet, for others, cannabis works as an alternative to ease some of the symptoms. Let’s take a look at why cannabis might be a suitable option for some people.
Cannabis For Anxiety: An Overview
The cannabis plant produces a plethora of unique phytochemicals—among these are over 100 cannabinoids and over 200 terpenes. Different strains and extracts contain varying concentrations of these chemicals and therefore produce different effects. Although touted as a “drug”, the complexity of cannabis chemistry eclipses this term. The terpene and cannabinoid profile of one strain can produce psychoactive effects entirely different from another cultivar.
Research in the field has revealed that cannabinoids and terpenes synergise to enhance and modify each other’s effects—a phenomenon known as the entourage effect[2]. Many of these molecules may affect anxiety symptoms in different ways, and certain strains and extracts might eventually work well for different people.
Let’s take a look at some of the most well-understood cannabinoids and terpenes below to see how they might combat or give rise to anxiety.
Types of Anxiety
- Generalised anxiety disorder
- People with this condition experience constant feelings of anxiety. Several causes underpin the condition, including an imbalance of brain chemicals, painful health conditions, and a history of drug and alcohol misuse.
- Obsessive-compulsive disorder
- Severe cases of this chronic disorder significantly impact the quality of life. The signs and symptoms include extreme fear of germs, unpleasant intrusive thoughts, aggression towards self and others, and the need for perfect order.
- Social phobia
- A long-term and overwhelming fear of social situations. The condition usually starts in people during their teenage years. The symptoms include worrying about everyday activities, frequently blushing and sweating, and a fear of embarrassment.
- Panic disorder
- Characterised by sudden and regular bouts of panic and fear. The causes of this condition include an imbalance of neurotransmitters and stressful life events. The symptoms include but aren't limited to nausea, chest pain, elevated heartbeat, trembling, and hot flushes.
- Post-traumatic stress disorder
- Traumatic events trigger this mental health condition. When people struggle to cope after such a situation, they may experience flashbacks, nightmares, and extreme anxiety.
THC Underpins The Cannabis High
THC underpins the quintessential psychoactive effectassociated with cannabis. It does so by binding to CB1 receptors in the brain, which causes a wave of dopamine and other neurotransmitters to surge.
Generally, the more THC a person consumes, the higher they feel. Breeders spent most of the last few decades selectively breeding cultivars to produce high levels of this cannabinoid. Some of the positive effects of THC that one may consider include:
| Euphoria | Creativity | Increased appetite | Relaxation |
| Euphoria | Creativity |
| Increased appetite | Relaxation |
These effects may help to ease anxiety in some cannabis users. However, new users and those sensitive to THC can experience effects that might increase their anxiety, making it worse in both the short- and long-term. These negative side effects may include:
| Anxiety | Paranoia | Confusion | Impaired short-term memory |
| Anxiety | Paranoia |
| Confusion | Impaired short-term memory |
So, THC can be a double-edged sword. Some users find great peace of mind when using high-THC strains, whereas others may experience worsening symptoms. Moreover, research[3] shows that low doses of THC can help to quell anxiety, whereas higher doses can cause it to spike. For this reason, it makes sense to use moderate to low-strength strains. This is why breeders have started creating cultivars that possess lower levels of THC and higher quantities of non-intoxicating cannabinoids, such as CBD.
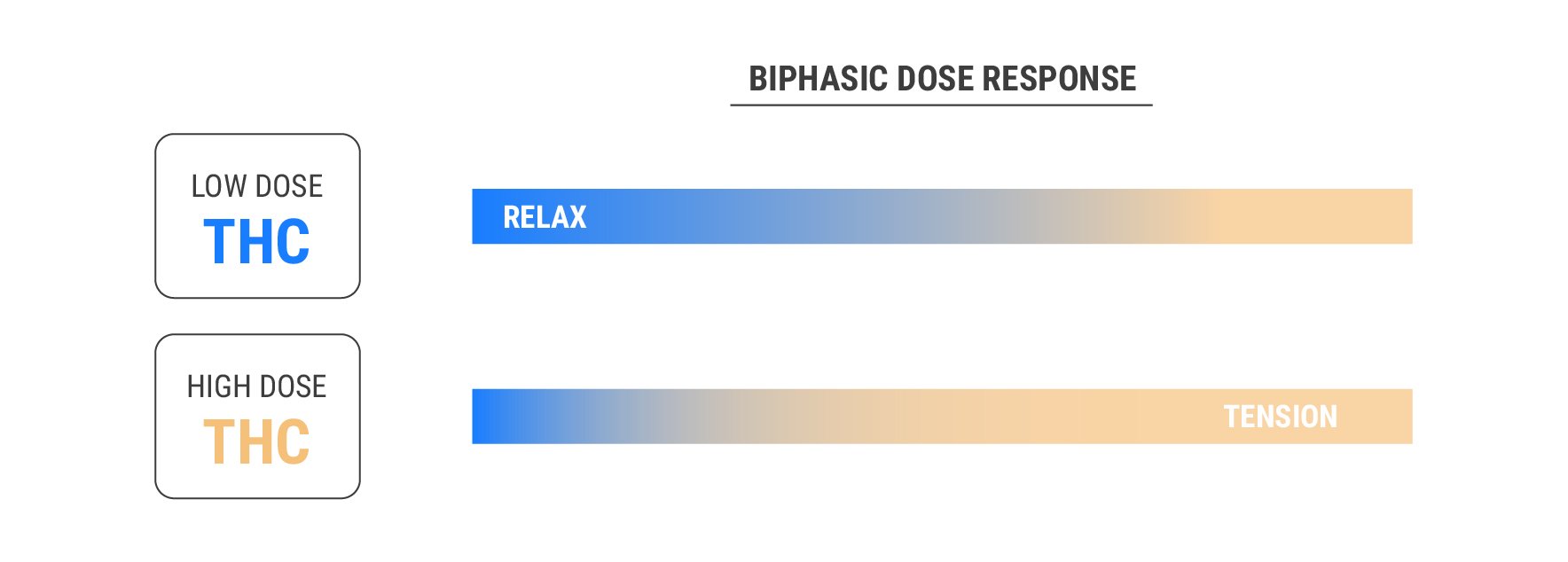
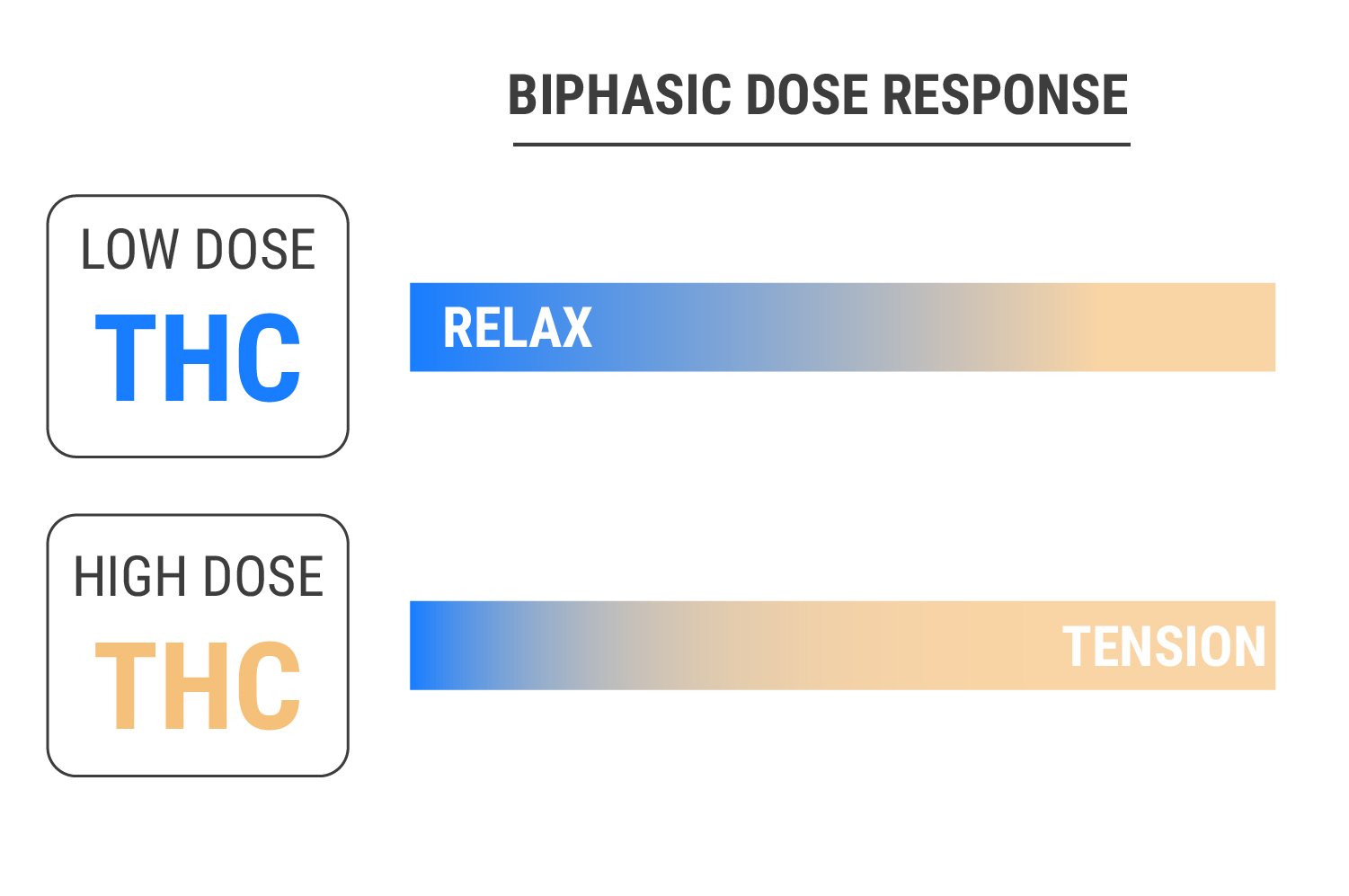
THC and the Biphasic Dose Response
New cannabis users have a lot of questions. They often ask, “how many milligrams of THC do you need to feel relaxed?”, or more simply, “how much THC gets you high?”. It turns out the answers to these questions are nuanced and more complex than you might think.
Ongoing trials have thus far found THC to exert a biphasic dose response. Put simply, this means it produces a certain effect at a low dose, and an opposite effect at a high dose.
Research conducted at the University of Illinois in 2017 found that this principle also applies to THC in the context of anxiety[4]. In order to explore the relationship between cannabis and anxiety, researchers recruited 42 healthy volunteers. Aged 18–40, the participants had some experience with the herb but weren’t regular users.
They randomly divided the subjects into three groups. The low-dose group received 7.5mg of THC, the moderate-dose group received 12.5mg of THC, and the placebo group received no THC. The double-blind nature of the study ensured that both the participants and the researchers remained unaware of who received what dose.
During the experiment, the researchers measured their blood pressure, heart rate, and cortisol levels. Interestingly, the participants who received the lower dose experienced less tension, and their tension levels dissipated faster. In contrast, the moderate-dose group experienced a negative mood before and during the programmed tasks.
These results suggest that THC causes a biphasic dose response in terms of anxiety. Lower doses appear relaxing, whereas higher doses seem to cause more tension. However, THC affects people differently, and our unique endocannabinoid tone and genetic expression mean we all experience the herb in our own ways. Moreover, this study focused on isolated THC. Cannabis flowers contain other phytochemicals that synergise with or antagonise the molecule, potentially making it possible for each person to tolerate higher doses of THC differently.
Does Weed Cause or Alleviate Social Anxiety?
Cannabis has a complex effect on the human brain. Every time you hit a blunt, bong, or joint, you’re inhaling an array of compounds that light up different binding sites, including cannabinoid, GABA, or serotonin receptors. Several cannabinoids and terpenes in the plant also interact with enzymes and pathways that influence mood and memory.
There are hundreds of cannabis chemovars available, all of which offer varying levels of different phytochemicals. Each person also has a unique physiology, which means all of these chemovars will affect each person slightly differently. Both the chemical complexity of the cannabis plant and the physiological diversity of people mean many variables are at play when considering the relationship between weed and anxiety.
After hitting a joint, some people are left asking, “Why does smoking weed make me socially anxious, nervous, and awkward?”. In contrast, some people become considerably more chatty and sociable after using cannabis. Let’s take a deeper look at what could be behind this.
Social Anxiety vs Anxiety: How Are They Different?
Social anxiety disorder autumns under the umbrella term of “anxiety”; however, it differs from other forms in that it involves a specific overwhelming fear of social situations. While most people get slightly nervous before public speaking or meeting a date for the first time, those with social anxiety disorder experience intense fears of daily social interactions.
People with social anxiety disorder experience emotional and behavioural symptoms including:
- Fear of embarrassment
- Intense fear of interacting with strangers
- Avoidance of speaking in public
- Fear of others perceiving symptoms of anxiety
- Expectations of the worst outcomes in social situations
As well as emotional symptoms, people with social anxiety also experience physical symptoms such as:
- Elevated heart rate
- Blushing
- Sweating
- Trembling
- Muscle tension

Several factors are thought to contribute toward social anxiety disorder, including:
- Genetics: Inherited traits may predispose some people to the condition.
- Brain structure: People with an overactive amygdala (a region involved in the fear response) may experience increased anxiety in social settings.

- Environment and previous experiences: Some people may develop social anxiety disorder following a distressing social event, such as extreme embarrassment during childhood.


Current Treatment for Social Anxiety
There is a range of treatment options available for people experiencing social anxiety disorder, including pharmaceutical and non-pharmaceutical routes. These include:
- Cognitive behavioural therapy (CBT): This form of therapy helps people to identify and change negative thought patterns.
- Antidepressant medications: Selective serotonin reuptake inhibitors (SSRIs), such as escitalopram, are prescribed to improve mood.
- Anti-anxiety medications: Benzodiazepines can help to reduce levels of anxiety.
- Beta blockers: These drugs block the action of adrenaline and minimise symptoms such as shaking and sweating.
Does Cannabis Cause Social Anxiety Disorder?
Can weed cause social anxiety? Some people report experiencing symptoms of the condition after using cannabis, both acutely and chronically. THC, the main psychoactive component of cannabis, binds to a site in the central nervous system called CB1. Through this mechanism, cannabis might stimulate or exacerbate social anxiety. Let's take a deeper look at how exactly this might occur.
- Amygdala overstimulation: Under normal conditions, endocannabinoids bind to CB1 receptors in the brain. The phytocannabinoid THC does the same, but it activates these sites much more intensely than normal. This can overstimulate receptors located on amygdala cells, resulting in paranoia and subsequent social anxiety.
- Dopamine blunting: Acutely, THC causes a rise in dopamine and sensations of euphoria in many cannabis users. However, over time, the molecule can lower levels of dopamine[5] in the brain. Social phobia may also arise from a long-term reduction[6] in dopamine receptor binding.
Does Cannabis Help Social Anxiety Disorder?
While some people are fraught with anxiety after hitting a joint, others find themselves much more social and less nervous. But why does this happen? Researchers are still looking into it, but it could involve the following:
- The biphasic dose response: While high levels of THC can stoke anxiety, lower doses are thought to create the opposite response[7].
- CB1 receptor activation: Anti-anxiety medications produce some of their effects through interactions with the CB1 receptor[8]. THC likely helps some people feel less nervous through this pathway.
- CBD: Many modern chemovars contain higher levels of CBD, a non-psychotropic cannabinoid that researchers are pitting against anxiety[9] in human studies.
- Terpenes: Cannabis also contains aromatic molecules known as terpenes. Scientists are working to find out if they synergise with cannabinoids to impact mood and anxiety[10].
The relationship between cannabidiol and anxiety
A lack of studies means that scientists can't make any conclusions just yet. But many interesting investigations are underway that will hopefully clear up the relationship between CBD and anxiety. Some of the most important ongoing studies include:
- How CBD affects ECS enzymes: Researchers are testing CBD for its ability to inhibit an ECS enzyme[5] known as fatty acid amide hydrolase (FAAH). This protein breaks down the endocannabinoid known as anandamide, which plays an important role in mood. If CBD helps prevent FAAH from breaking it down, it could have a knock-on effect on mental state.
- The link between CBD and GABA: Ongoing studies are also looking into how CBD affects GABA levels[11] in the brain. Also known as gamma-aminobutyric acid, this inhibitory neurotransmitter works to dampen brain activity, which helps to turn things down a notch in the anxious brain.
- Testing CBD against social anxiety: Researchers are now conducting human experiments to see how CBD influences certain outcome measures. For example, a paper published in the journal Neuropsychopharmacology administered CBD to patients with generalised anxiety disorder before engaging in a simulated public speaking event[12]. The researchers looked to measure factors such as cognitive impairment, discomfort, and levels of alertness.
- CBD and blood flow to the brain: Some human studies are taking things a step further and looking to see if CBD alters blood flow to regions of the brain associated with anxiety. Using arterial spin labelling (an MRI technique that measures changes in blood oxygen levels), a team of University College London set out to see if CBD changes blood flow to the hippocampus[13]—a brain region associated with the modulation of anxiety.
Does CBD Produce Anxiety?
CBD produces side effects in some users, including nausea, fatigue, and irritability. The cannabinoid can also interact with a long list of prescribed medications. However, the cannabinoid isn't known to induce anxiety at this time.
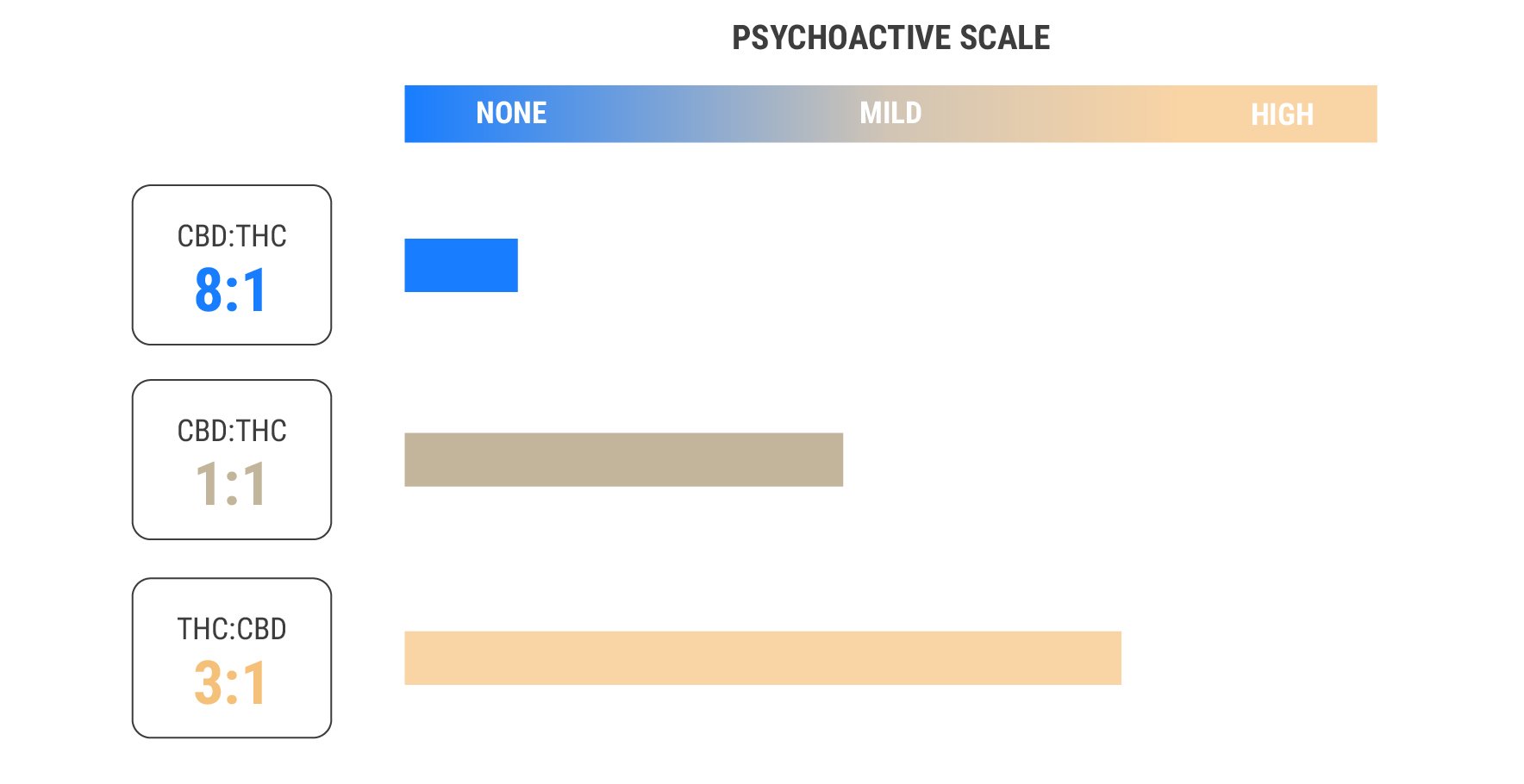
Using THC And CBD Together
CBD could produce a clear-headed and relaxing sensation without any inhibiting psychoactive effects. Therefore, if users decide to try cannabis against anxiety, CBD is more of a feasible option than THC for many anxiety sufferers. However, people could potentially benefit from both cannabinoids at the same time.
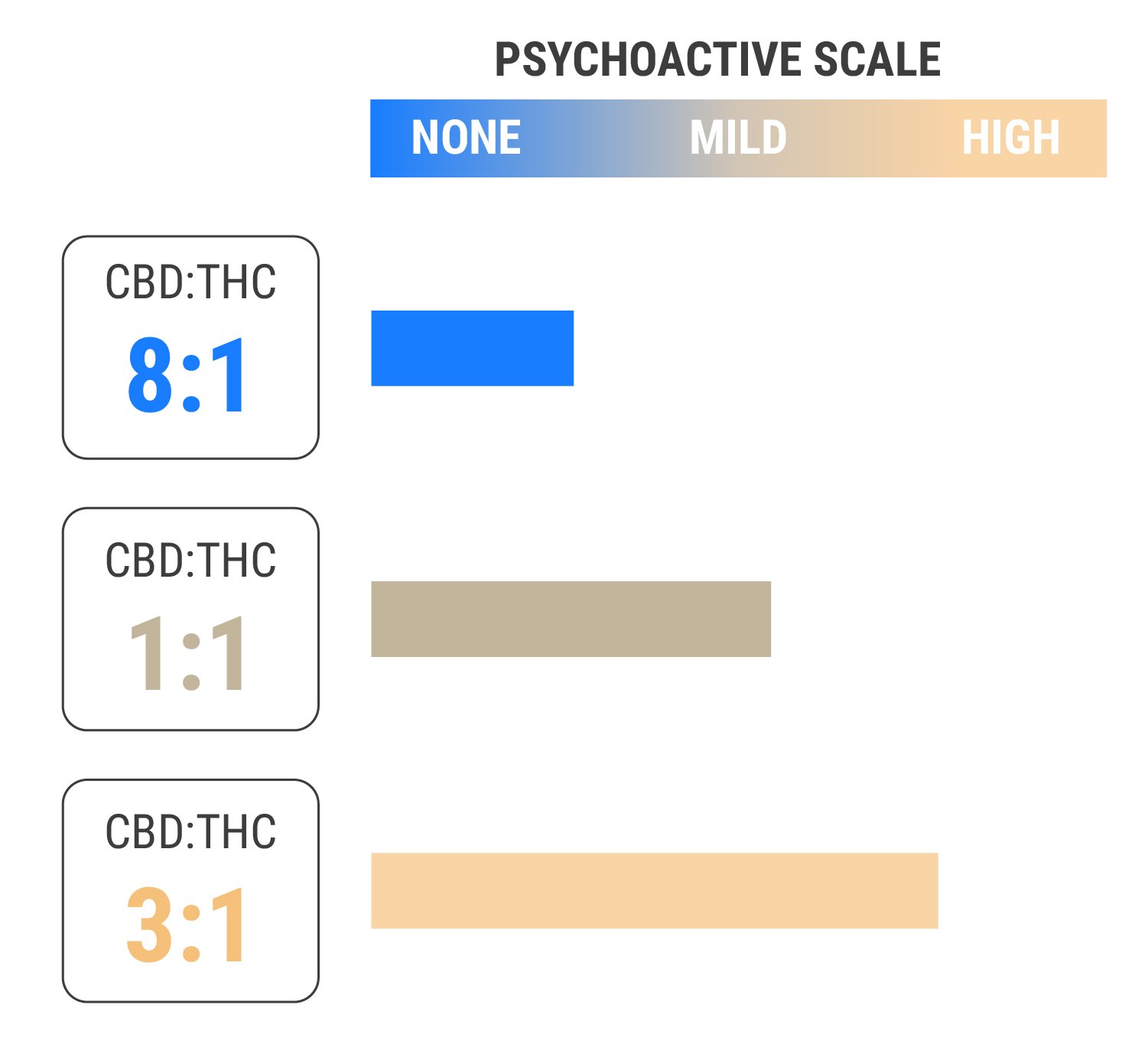
Some strains contain varying ratios of the two chemicals. CBD:THC ratios of 1:1 provide a balanced effect, whereas ratios of 8:1 or higher provide almost no psychoactive effects at all. Interestingly, CBD appears to block THC at the CB1 receptor[15], meaning it might help to reduce the intensity of THC. These findings suggest that those sensitive to THC might experience its benefits when using CBD at the same time.
Terpenes Matter
If THC and CBD exist in most strains, why do different cultivars produce different effects? Although these cannabinoids largely underpin cannabis’ effects, terpenes add a unique spin that makes each strain different. Just like cannabinoids, terpenes offer their own unique pharmacology. If you decide to try the herb against anxiety, be sure to check out the terpene profile of a strain before you consume or cultivate it.
Below are some of the most promising terpenes when it comes to anxiety:
- Myrcene: The most abundant terpene in most cannabis strains, myrcene features an earthy, musky scent. It also heavily contributes to the stoning high of many indica varieties. The terpene exerts sleep-promoting effects that might help to improve sleep quality and relax the body. Via the entourage effect, myrcene may increase the soothing properties[15] of THC.
- Limonene: This terpene adds a citrusy scent to cannabis flowers. Strains high in limonene literally taste like oranges and lemons! In animal studies[16], the molecule has demonstrated an ability to boost serotonin and dopamine. Limonene also appears to enhance the anxiolytic action[17] of CBD.
- Caryophyllene: Both a terpene and a dietary cannabinoid, caryophyllene binds to the CB2 receptor of the endocannabinoid system. Caryophyllene imparts a peppery, spicy taste, and has produced anxiolytic[18] effects in animal models.
- Pinene: Responsible for the fresh smell of pine, pinene unleashes an earthy and piney aroma. The terpene has demonstrated an anxiolytic effect in animal studies[19], and it may help to counteract some of the negative side effects of THC, such as short-term memory impairment.
Timing Is Important
If you decide to try cannabis against anxiety, it is important to choose which strain and mix of phytochemicals works best for you. From here, you must decide the best time to take it. Not much data exists on timing, so you’ll have to find what works best through trial and error.
For some users, taking CBD-rich cannabis in the morning might help keep their anxiety low throughout the day. Others might find it more helpful to take extracts or hit a joint right as their symptoms begin to occur. For those who have trouble sleeping, enjoying an indica strain rich in THC and myrcene before bed may help them wind down.
Remember, different products take effect at different times. Edibles take an hour or more to set in, but the effect lasts longer. Vaping and sublingual administration work much faster, but the effects are more transient.
Many users also find great success with microdosing, which involves taking a sub-perceptual amount of cannabis in order to address symptoms without feeling high.
Cannabis and Psychotherapy: Are They Compatible?
Cannabis may contribute to or worsen mental health conditions in susceptible individuals, but some find the herb to actually work alongside psychotherapy.
What Is Psychotherapy?
Psychotherapy is a form of talk therapy. During sessions, psychotherapists help patients to understand their symptoms, feelings, thoughts, and behaviours. Practitioners use a range of techniques to achieve this, including cognitive behavioural therapy (CBT) and dialectical behaviour therapy (DBT). These strategies can help with a range of conditions, including anxiety, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD).
Does Cannabis Have a Place in Psychotherapy?
Under certain circumstances, psychotherapy and medications are used to achieve better patient outcomes. But do weed and therapy go hand in hand? No studies have sought to determine how cannabis impacts the success of psychotherapy sessions. However, many people experiencing various health conditions use cannabis to experience the plant’s holistic benefits. Researchers have found that some cannabis users would expect cannabis-assisted psychotherapy[20] to help them deal with depression. The same expectations could be true for anxiety. In any case, it’s clear that using cannabis in psychotherapy is in demand among some people.
The Future of Cannabis-Assisted Psychotherapy
Is there a place for marijuana in psychotherapy? As psychedelic-assisted psychotherapy starts to edge its way into the mainstream, we could see cannabis used in a similar context in the future. Right now, the herb remains understudied. Researchers are just getting to grips with how certain molecules influence human neurochemistry, and how they might help to improve some conditions. As we continue to uncover the vast chemical complexity of the cannabis plant, we could find more molecules fit for cannabis-assisted therapy.

Cannabis Can Help, But Shouldn’t Be A Crutch
Cannabis can make a big difference in some anxiety sufferers, but it shouldn’t be overused or relied upon. However, it can form part of a wider approach. Diet, meditation, therapy, exercise, and communication all play an important role in such a strategy. Balance is the key.
Which Cannabis Strain To Choose?
If you decide to try cannabis, we think the following three strains cover the most bases when using cannabis as a means of managing anxiety. It is impossible to say how you will react when consuming cannabis but understanding the different effects that can be obtained will help you to make an educated and informed judgement. Finally, starting with a low THC and/or high CBD strain is more than likely the best place for most anxiety sufferers. CBD is a non-psychoactive compound that can help combat anxiety with attributes such as a clearer head and a stronger feeling of calm.
Stress Killer
Kicking things off you couldn't get a more apt name. Whilst primarily a sativa dominant strain, it still possesses a strong indica pairing. Sativa strains typically uplift and energise the user which can be detrimental when trying to calm oneself. Stress Killer mixes the best of both worlds. It has a THC content of 11%, whilst also being high in CBD to provide that clear head high. Bursting with citrusy flavours, this is a surefire strain to kick start your day.

Stress Killer Automatic CBD
|
|
Lemon Shining Silver Haze x Juanita la Lagrimosa x Ruderalis |
|
|
450 - 500 gr/m2 |
|
|
90 – 140 cm |
|
|
7 - 8 weeks |
|
|
THC: 11% |
|
|
Sativa 60% Indica 30% Ruderalis 10% |
|
|
110 - 160 gr/plant |
|
|
120 – 160 cm |
|
|
11 - 12 weeks after sprouting |
|
|
Clear, Focus |
Buy Stress Killer Automatic CBD
Royal Jack Automatic
Named after a tireless cannabis activist, Jack Herer. Royal Jack Automatic, whilst still slightly sativa dominant is a more balanced strain. Because of the higher indica DNA, it gives a slightly more body stoned feeling to help when that anxiety starts to build and you need some time to yourself. Despite this, a medium CBD content still helps to keep things clear so you can think with renewed clarity.

Royal Jack Auto
|
|
Jack Herer x Ruderalis |
|
|
350 - 400 gr/m2 |
|
|
40 - 80 cm |
|
|
7 - 8 weeks |
|
|
THC: 16% |
|
|
Sativa 40% Indica 30% Ruderalis 30% |
|
|
70 - 120 gr/plant |
|
|
60 - 80 cm |
|
|
11 - 12 weeks after sprouting |
|
|
Creative, Motivating |
Northern Lights
Being an indica dominant hybrid, this strain is very much an end of the day affair. Boasting some award-winning genetics is provides a strong stone able to couchlock the user whilst they enjoy the high. Perfect for when some contemplation time is needed or for when the days events can become too much. Providing a medium strength of CBD it also has the highest THC content of all three strains.

Northern Light
|
|
Northern Light S1 |
|
|
500 - 550 gr/m2 |
|
|
100 - 160 cm |
|
|
8 - 9 weeks |
|
|
THC: 18% |
|
|
Sativa 0% Indica 100% |
|
|
575 - 625 gr/plant |
|
|
180 - 220 cm |
|
|
Late September |
|
|
Balanced, Clear, Stoned |
Finally, this list is by no means exhaustive. As every person is unique, so is their choice in weed. The better option is to start with less-psychoactive plants before you commit to a lengthy or powerful session. Typically, smoking or vaping allow you to control the high a lot more than dabs or edibles, so these methods of consumption are the better option to start with if you decide to give cannabis a chance against anxiety
- Facts & Statistics | Anxiety and Depression Association of America, ADAA https://adaa.org
- Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects - PMC https://www.ncbi.nlm.nih.gov
- https://www.sciencedaily.com/releases/2017/06/170602155252.htm
- https://www.sciencedaily.com/releases/2017/06/170602155252.htm
- Cannabidiol as a Potential Treatment for Anxiety Disorders | SpringerLink https://link.springer.com
- Psychiatry Online https://ajp.psychiatryonline.org
- Cannabis blunts the brain's reward system | Imperial News | Imperial College London https://www.imperial.ac.uk
- https://adai.uw.edu/pubs/pdf/2017mjanxiety.pdf
- The cannabinoid CB1 receptor is involved in the anxiolytic, sedative and amnesic actions of benzodiazepines - PubMed https://pubmed.ncbi.nlm.nih.gov
- https://journals.sagepub.com/doi/abs/10.1177/0269881110379283
- The "Entourage Effect": Terpenes Coupled with Cannabinoids for the Treatment of Mood Disorders and Anxiety Disorders - PubMed https://pubmed.ncbi.nlm.nih.gov
- Cannabidiol as a Potential Treatment for Anxiety Disorders | SpringerLink https://link.springer.com
- Cannabidiol Reduces the Anxiety Induced by Simulated Public Speaking in Treatment-Naïve Social Phobia Patients | Neuropsychopharmacology https://www.nature.com
- https://journals.sagepub.com/doi/abs/10.1177/0269881110379283
- https://www.sciencedirect.com/science/article/abs/pii/S1054358917300273
- Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects - PMC https://www.ncbi.nlm.nih.gov
- https://www.sciencedirect.com/science/article/abs/pii/S1054358917300273
- Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects - PMC https://www.ncbi.nlm.nih.gov
- https://www.sciencedirect.com/science/article/abs/pii/S0031938414003400
- https://www.sciencedirect.com/science/article/abs/pii/S1054358917300273
- Expectancies for Cannabis-Induced Emotional Breakthrough, Mystical Experiences and Changes in Dysfunctional Attitudes: Perceptions of the Potential for Cannabis-Assisted Psychotherapy for Depression | Cannabis https://www.publications.sciences.ucf.edu