.

Should You Consume CBD While on Medication?
Can you use CBD oil while taking medication? How does the cannabinoid interact with substances in the body? We have the answers you're looking for.
Contents:
One of the oft-asked questions in regards to health and pharmaceuticals is whether or not cannabis can be mixed with medication. It is, indeed, a valid concern to raise, especially for those who regularly take cannabidiol for whatever purpose. It is understandable that some to argue in support of it, especially when it comes to CBD oil. After all, it’s non-psychotropic and used by thousands every single day, so it should be safe, right?
Well, in case you didn't know, the cannabis plant contains over a hundred chemical compounds. Some of these compounds can react with one another, which cannot be perceived as a major health problem. But the question is, will occur an innocuous reaction when it comes to CBD interacting with other drugs?
This article should provide you with a clear answer, once and for all. Hopefully, the information will be helpful for you down the line.
Can CBD Oil Affect Medication?
Before answering this, let’s first address another important question: how exactly does CBD interact with our bodies?
There is not a simple answer, but basically: CBD interfaces with the main receptors in the endocannabinoid system—CB1 and CB2—among other molecular targets, including serotonin and vanilloid receptors. Intriguingly, CBD hinders the breakdown of certain chemicals—including anandamide—that directly affect our mood, pain perception, or some mental functions, such as memory.
In doing so, CBD is able to modify the homeostasis (dynamic balance) between our physiological systems. Therefore, the use of CBD-rich cannabis strains or CBD derivates could be beneficial for some individuals under some delimitated situations.
However, is important to know that CBD also affects the metabolism of medications, a process that takes place primarily in the liver.
How Does the Body Metabolise CBD?
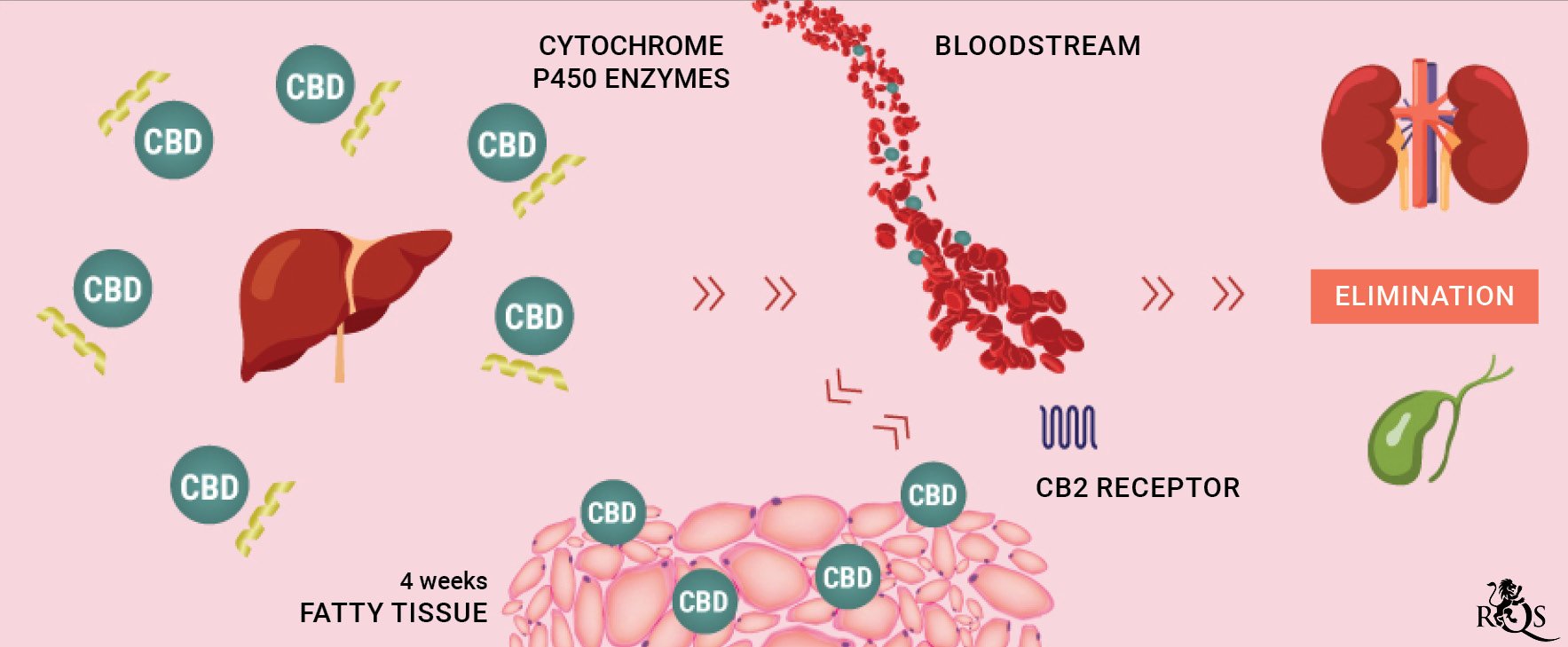
CBD's interactions with other drugs largely stem from their common metabolising process and effects produced in the cytochrome P450 system. This group of liver enzymes (isoenzymes) is mainly responsible of modifying toxins, drugs, and other substances in our system. These enzymes basically alter these substances to make them easier to eliminate from the body.
But when CBD enters the body, the liver may reduce the metabolising rate of other drugs that also rely on cytochrome P450 enzymes.
In some cases, CBD can almost completely block cytochrome P450 activity, albeit temporarily, affecting the metabolic activity of compounds found in certain drugs. So, for example, if you’re taking a powerhouse painkiller like oxycodone alongside cannabidiol (CBD), the former may linger in your system for longer and in higher concentrations than expected—which isn’t necessarily a good thing.
What can be problematic is that a drug like oxycodone is only supposed to stay in your system in determinate amounts for a certain period of time. Going beyond that duration may elicit overdoses or increase side effects like nausea and drowsiness. All of this could be an issue if you’re driving a car or operating heavy machinery. At worst, these interactions can also cause other damage to your body.
Depending on the dose and method of administration, CBD can remain in the body for about four weeks. During that time, it is stored within fatty tissues until it is gradually released in small doses back into the bloodstream. From there, cannabidiol is excreted from the body through the renal (aka urinary) and biliary systems.
Now, we mentioned cytochrome P450 enzymes and the vital role they play in metabolising CBD. But, what are they exactly?
.jpg)
What Is the Cytochrome P450 System?
CBD's interactions with other drugs largely stem from their common metabolizing process and effects produced in the cytochrome P450 system. This group of liver enzymes (isoenzymes) is mainly responsible of modifying toxins, drugs, and other substances in our system. These enzymes basically alter these substances to make them easier to eliminate from the body.
But, when CBD enters the body, the liver may reduce the metabolising rate of other drugs that also rely on cytochrome P450 enzymes.
Albeit temporarily, in some cases, CBD can almost completely block the cytochrome P450 activity, affecting the metabolic activity of compounds found in certain drugs. So, for example, if you’re taking a powerhouse painkiller like oxycodone alongside cannabidiol (CBD), the former may linger in your system for longer and in higher concentrations than expected— which isn’t necessarily a good thing.
What can be problematic is that a drug like oxycodone is only supposed to stay in your system in determinate amounts for a certain period of time. Going beyond that duration may elicit overdoses or increase of side effects like nausea and drowsiness. All this could be an issue if you’re driving a car or operating heavy machinery. At worst, these interactions can also cause other damages to your body.
Drugs CBD Oil Can Interact With
The fact of the matter is, cytochrome P450 enzymes metabolise around 90%[1] of all medications on the market, with two izoenzymes in particular—CYP3A4 and CYP2D6—being responsible for the lion’s share of the work. So, here’s a simplified answer: almost any drug metabolised by cytochrome P450 enzymes will interact with CBD oil. Some of these drug interactions will bear no notable adverse effects, while others will.
Let’s get a little more specific. A 2016 study[2] delved into how CBD reacted with a known anti-seizure medication called clobazam, which is largely used to treat epilepsy among children. This interaction is particularly intriguing, as CBD (in synthetic form, "Epidiolex") has also been approved for treatment-resistant forms of Lennox–Gastaut syndrome and Dravet syndrome.
The study found that cannabidiol slowed down the metabolism of clobazam, which led to a significant increase in plasma levels of medication in the body—around 60–80%. As a result, researchers were able to lower the dose of clobazam administered to the subjects, without sacrificing efficacy. Even more interesting, the drug’s side effects, like insomnia, loss of coordination, drowsiness, and constipation, were all curbed with this lower dose.
Basics of Pharmacodynamics and CBD-Drug Interaction: Examples
A substrate is any substance modified by an enzyme. In respect to drugs, there are two kinds of substrates: ones that are already active when they are ingested, which are simply called drugs (for example, THC, the main compound of cannabis), and ones that must first be metabolised in order to become active, which are called prodrugs (for example, psilocybin, which is the prodrug of psilocin, the main active component of “magic mushrooms”).
These substrates usually do not affect the normal activity of the enzyme that metabolises them. However, there exist other substances that can increase the metabolic activity of cytochrome P450 enzymes: enzymatic inducers. There are also others that can reduce or even block normal enzymatic activity, known as enzymatic inhibitors. All of them can interact with one another, too.
| Kind of substrate | Drug | Pro-drug |
| Effect when combined with an enzymatic inhibitor (including CBD) | Increase | Reduction |
| Effect when combined with an enzymatic inducer | Reduction | Increase |
| Effect when combined with an enzymatic inducer + CBD | Variable | Variable |
| Kind of substrate | Drug | Pro-drug |
| Effect when combined with an enzymatic inhibitor (including CBD) | Increase | Reduction |
| Effect when combined with an enzymatic inducer | Reduction | Increase |
| Effect when combined with an enzymatic inducer + CBD | Variable | Variable |
Also included are some considerations on whether or not cannabidiol should be used.
CYP3A4 Substrates
CYP3A4, specifically, is an liver and intestines isoenzyme forming part of the cytochrome P450 that oxidises toxins or drugs for easier excretion from the body.
Some Iimmunosuppressants and antidepressants alongside antipsychotics, calcium channel blockers, and opioids are substrates of this isoenzyme. Also part of these substrates are benzodiazepines, z-hypnotics, statins, and chemotherapeutics.
The risk of side effects, loss of effect or on the contrary, overdose may be increased when in co-administration with CBD – an enzymatic inhibitor. The safest situation is to not combine these drugs until receiving an expert recommendation.
| Amlodipine | Sinvastatin |
| Haloperidol | Citalopram |
| Fentanyl | Cabazitaxel |
| Zolpidem | Tacrolimus |
| Amlodipine | Sinvastatin | Haloperidol | Citalopram |
| Fentanyl | Cabazitaxel | Zolpidem | Tacrolimus |
CYP34 Inhibitors
Protease inhibitors are antiviral drugs that are usually prescribed to patients diagnosed with HIV. Valproic acid, on the other hand, is a medication used for epilepsy treatment.
These drugs are examples of CYP3A4 inhibitors, and they are quite similar to their substrate counterparts.
When CBD interacts with any of these drugs, its bioavailability—or the bloodstream drug concentration —tends to increase. As a result, the risk of adverse effects may rise.
Experts don’t advice taking CBD alongside these medications, but a reduced dose is recommended, should you decide to combine both medications.
Protease inhibitors and valproic acid are examples of stronger CYP34 inhibitors. Other ones are amiodarone, verapamil, aprepitant, and cimetidine.
| Allopurinol | Fluconazole |
| Amiodarone | Fluoxetine |
| Amprenavir | Quinolones |
| Aprepitant | Valproic acid |
| Atazanavir | Erythromycin juice |
| Chloramphenicol | Imatinib |
| Cimetidine | Indinavir |
| Clarithromycin | Isoniazid |
| Nifedipedine | Itraconazole |
| Tamoxifen | Ketoconazole |
| Cyclosporine | Nefazodone |
| Darunavir | Nelfinavir |
| Dasatinib | Ritonavir |
| Delavirdine | Verapamil |
| Diltiazem | Saquinavir |
| Allopurinol | Chloramphenicol | Cyclosporine | Erythromycin | Imatinib | Nefazodone |
| Amiodarone | Cimetidine | Darunavir | Fluconazole | Indinavir | Nelfinavir |
| Amprenavir | Clarithromycin | Dasatinib | Quinolones | Isoniazid | Ritonavir |
| Aprepitant | Nifedipedine | Delavirdine | Valproic acid | Itraconazole | Verapamil |
| Atazanavir | Tamoxifen | Diltiazem | Fluoxetine | Ketoconazole | Saquinavir |
CYP3A4 Inducers
Barbiturates are medications used to treat people suffering from seizures.
In this case, increasing the dose of cannabidiol might seem logical; however, this idea should not be pursued due to the intrinsic risks of overdose and side effects when combining CBD with some medications.
Other examples of CYP3A4 inducers are detailed in the following table.
| Carbamazepine | Omeprazole |
| Corticosteroids | Rifampin |
| Efavirenz | Oxacarbazepine |
| Rifabutin | Phenytoin |
| Modafinil | Primidone |
| Nevirapine | St. John's wort |
| Carbamazepine | Efavirenz | Modafinil | Omeprazole | Oxacarbazepine | Primidone |
| Corticosteroids | Rifabutin | Nevirapine | Rifampin | Phenytoin | St. John's wort |
CYP2C19 Substrates
The CYP2C19 isoenzyme metabolises xenobiotics like anti-seizure medications. And, like CYP34 substrates, they could carry some side effects when mixed with CBD.
Similarly, co-administration with cannabidiol isn’t advised, and adverse effects and toxicity need to be monitored closely.
Other examples of CYP2C19 substrates are proton pump inhibitors, antidepressants, antiplatelet drugs, muscle relaxants, and blood thinners.
| Aripiprazole (Abilify) | Lansoprazole (Prevacid) |
| Carisoprodol (Soma) | Mephenytoin (Mesantoin) |
| Citalopram (Celexa) | Methadone |
| Clomipramine (Anafranil) | Propranolol |
| Clopidogrel (Plavix) | Voriconazole (Vfend) |
| Clozapine (Clozaril) | R-warfarin |
| Desipramine (Norpramin) | Moclobemide (Manerix) |
| Diazepam (Valium) | Nelfinavir (Viracept) |
| Sertraline (Zoloft) | Olanzapine (Zyprexa) |
| Thalidomide | Omeprazole (Prilosec) |
| Proguanil | Pantoprazole (Protonix) |
| Diphenhydramine (Benadryl) | Pentamidine |
| Doxepin (Sinequan) | Phenobarbital |
| Escitakopram (Lexapro) | Phenytoin |
| Fluoxertine (Prozac) | Rabeprazole |
| Imipramine (Tofranil) |
| Allopurinol | Desipramine (Norpramin) | Diphenhydramine (Benadryl) | Lansoprazole (Prevacid) | R-warfarin | Pantoprazole (Protonix) |
| Carisoprodol (Soma) | Diazepam (Valium) | Doxepin (Sinequan) | Mephenytoin (Mesantoin) | Moclobemide (Manerix) | Pentamidine |
| Citalopram (Celexa) | Sertraline (Zoloft) | Escitakopram (Lexapro) | Methadone | Nelfinavir (Viracept) | Phenobarbital |
| Clomipramine (Anafranil) | Thalidomide | Fluoxertine (Prozac) | Propranolol | Olanzapine (Zyprexa) | Phenytoin |
| Clopidogrel (Plavix) | Proguanil | Imipramine (Tofranil) | Voriconazole (Vfend) | Omeprazole (Prilosec) | Rabeprazole |
| Clozapine (Clozaril) |
CYP2C19 Inhibitors
Those who use anxiolytics may be familiar with fluoxetine. It is also used to treat specific mental conditions like depression and even bulimia. Similarly, fluvoxamine is an antidepressant that is mainly used by people with obsessive-compulsive disorder.
These two drugs are primary examples of CYP2C19 inhibitors. As it is with these medications, CBD’s bioavailability could potentially increase. The risk of adverse effects may rise as a result, which is why lower CBD doses are advised, though drug combination avoidance is a better option.
| Chloramphenicol | Isoniazid |
| Cimetidine (Tagamet) | Moclobemide (Manerix) |
| Clopidogrel (Plavix) | Modafinil (Provigil) |
| Delavirdine (Rescriptor) | Omeprazole (Priosec) |
| Efavirenz (Sustiva) | Oxcarbazepine (Trileptal) |
| Esomeprazole (Nexium) | Ticlopidine (Ticlid) |
| Felbamate (Felbatol) | Voriconazole (Vfend) |
| Fluconazole (Prozac) | Fluconazole (Diflucan) |
| Fluvoxamine |
| Chloramphenicol | Clopidogrel (Plavix) | Efavirenz (Sustiva) | Felbamate (Felbatol) | Fluvoxamine | Moclobemide (Manerix) |
| Omeprazole (Priosec) | Oxcarbazepine (Trileptal) | Fluconazole (Diflucan) | Cimetidine (Tagamet) | Delavirdine (Rescriptor) | Esomeprazole (Nexium) |
| Fluconazole (Prozac) | Isoniazid | Modafinil (Provigil) | Ticlopidine (Ticlid) | Voriconazole (Vfend) |
CYP2C19 Inducers
Tuberculosis patients will be greatly familiar with rifampicine. It’s a oral medication used as an antibiotic to treat bacterial infections. Meanwhile, carbamazepine is an anticonvulsant used to treat seizures and neurological pain.
These two drugs are the best examples of CYP2C19 inducers. Theoretically, they could be safer when taken with CBD because, unlike inhibitors, the bioavailability of the cannabinoid decreases upon interaction, resulting in a reduction in effectiveness. In any case, it is not recommend to increase CBD dose if administered with CYP2C19 inducers.
| Aminoglutethimide | Primidone |
| Artemisinin | Rifampin |
| Barbiturates | Rifapentine |
| Carbamazepine | St. John's wort |
| Phenytoin |
| Aminoglutethimide | Barbiturates | Phenytoin | Rifampin | |
| Artemisinin | Carbamazepine | Primidone | Rifapentine | St. John's wort |
CYP2C8/9 Substrates
Both CYP2C8 and CYP2C9 enzymes are responsible for metabolising xenobiotics. However, the former can also metabolise polyunsaturated fatty acids.
Therefore, there is an increased risk of side effects when combined with CYP2C8/9 inhibitors. Co-administration with CBD isn’t advised, and using lower substrate doses to obtain the same CBD effect is not recommended.
A good example of a CYP2C8 and CYP2C9 substrate is rosiglitazone, a medication for type 2 diabetes. Antihypertensive drug losartan is also part of this list, along with naproxen, celecoxib, rosuvastatin, and sulfonylureas—just to name a few.
| Amiodarone (Cordarone) | Carbamazepine (Tegretol) |
| Diclofenac (Voltaren) | Paclitaxel (Taxol) |
| Repaglinide (Prandin) | Cabazitaxel (Jevtana) |
| Chloroquine (Aralen) | Ibuprofen (Advil) |
| Rosiglitazone (Avandia) | Treprostinil (Tyvaso) |
| Amiodarone (Cordarone) | Carbamazepine (Tegretol) | Diclofenac (Voltaren) | Paclitaxel (Taxol) | Repaglinide (Prandin) |
| Cabazitaxel (Jevtana) | Chloroquine (Aralen) | Ibuprofen (Advil) | Rosiglitazone (Avandia) | Treprostinil (Tyvaso) |
What Is the Grapefruit Test?
You’ve probably seen the “grapefruit warning” on some of your medications. If you’re taking one of these drugs, you’re advised to avoid consuming any grapefruit and other types of citrus. But why is that?
Like CBD, grapefruit and other citrus inhibits cytochrome P450 enzymes, which directly affects the metabolism of these substances. That means consuming grapefruit could modify the dose of the drug or the prodrug in the bloodstream, which may result in an overdose or reduction in drug efficiency.
Research shows that more than 85 drugs[3] share this same interaction with grapefruit. Among them are fentanyl, erythromycin, losartan, loratadine, and alprazolam.
If in Doubt, Speak to Your Doctor
So, with all the hype behind it, is it safe to take CBD oil while on medication? If you’ve read through the entire article, the most logical answer would be: it depends on what you are taking, the method of administration, and the dose.
Nothing good ever came from uninformed dosing or practising excessive use.
But, if you want to be on the safest side, ask your doctor. They can speak to you in lay terms about the effects of these drugs and how CBD may interact with them. This is the best way to obtain sound advice and answers to any questions you may have.
Medical DisclaimerInformation listed, referenced or linked to on this website is for general educational purposes only and does not provide professional medical or legal advice.
Royal Queen Seeds does not condone, advocate or promote licit or illicit drug use. Royal Queen Seeds Cannot be held responsible for material from references on our pages or on pages to which we provide links, which condone, advocate or promote licit or illicit drug use or illegal activities. Please consult your Doctor/Health care Practitioner before using any products/methods listed, referenced or linked to on this website.
- The Effect of Cytochrome P450 Metabolism on Drug Response, Interactions, and Adverse Effects - American Family Physician https://www.aafp.org
- Human Metabolites of Cannabidiol: A Review on Their Formation, Biological Activity, and Relevance in Therapy https://www.ncbi.nlm.nih.gov
- Common Grapefruit Juice Drug Interactions - Drugs.com https://www.drugs.com