.
Can You Smoke Weed While on Antibiotics?
Can you smoke weed while taking antibiotics? Does weed itself work as an antibiotic? Join us as we take a deep dive into the history and types of antibiotics, if cannabinoids such as THC and CBD interact with them, and if cannabis has a place in the future of treating antibiotic-resistant strains of bacteria.
Key Takeaways
- THC and CBD can inhibit liver enzymes (CYP450) and affect antibiotic metabolism.
- Evidence on THC–antibiotic interactions is limited, with isolated reports.
- CBD may pose a higher interaction risk by increasing side effects.
- Smoking during a respiratory infection can worsen symptoms.
- Cannabinoids are being studied as antibacterials, but evidence remains preclinical.
Contents:
- The relationship between marijuana and antibiotics: two approaches
- The importance of antibiotics
- The different types of antibiotics
- Can you smoke weed on antibiotics?
- What is antibiotic resistance?
- Is marijuana a potential antibiotic?
- What about other antibacterial cannabinoids?
- The future for cannabis as an antibiotic
Can you smoke weed on antibiotics? Considering millions of people use cannabis every day, and millions of doses of antibiotics are also taken daily, it’s worth knowing if an interaction exists between the two.
However, the relationship between cannabis and antibiotics may go deeper than simple drug interactions.
Early studies are examining the antibiotic potential of cannabis compounds in hopes of finding novel weapons against drug-resistant strains of bacteria.
Below, you’ll find out if it’s safe to smoke weed while on antibiotics. Then, we’ll delve into the antibacterial potential of cannabis compounds to see if the plant might have a place in the future of antibiotic medicine.
The Relationship Between Marijuana and Antibiotics: Two Approaches
First of all, cannabis users should know whether they are putting their health at risk if they take cannabis and prescription antibiotics at the same time. After all, cannabis does interact negatively with some drugs.
Cannabis itself might be an intriguing target in the search for antibiotic-like substances capable of combating drug-resistant strains of bacteria.
Consider for a moment how lucky we are in the modern era. Sure, many of us experience the stress of deadlines, bills, and overstimulation. But we often take for granted how humans have transcended the throes of tooth and claw that our ancestors endured. Nature is a cycle of life and death; an ongoing war between countless species. One of our oldest enemies—bacteria—could have ended us in the past, but we’re now lucky enough to have access to pills that kill it off.
Antibiotics save over 200,000 lives each year in the United States alone. But humans aren’t the only species with a tendency to adapt and overcome; species of bacteria are mutating and developing resistance. Now, researchers are eyeing up new sources of antibiotics to counter this threat—some have placed cannabis in the crosshairs.
The Importance of Antibiotics
Antibiotics are an essential weapon in the age-old war against microbial life. Of course, not all microscopic organisms inflict disease; the human gut contains trillions of bacteria, fungi, and viruses that help us to digest food and bolster our immune system. But many other species of microbes don’t work in such a symbiotic manner with the human body.
There are myriad species and strains of infectious bacteria. These organisms can work their way into the human body through various means, including contact, airborne, and droplet transmission. For example, eating a poorly cooked piece of food often serves as the entryway for some species.
However, infections can occur at any site in the body. The symptoms either arise from the bacteria itself, or the body's reaction to its presence. Bacteria vary in their pathogenicity (their potential to cause disease); only a small percentage of species cause infection and disease in humans, but many of these can cause serious damage.
Every organ in the human body is susceptible to bacterial infection. Species that attack the meninges (membranes that protect the brain and spinal cord) can cause meningitis. Those that go after the lungs can cause pneumonia. Staphylococcus aureus, which usually occupies the skin, can gain entrance to the body via wounds and infect the heart valves and abdomen.


-
A Brief History of Antibiotics
Thankfully, antibiotics have helped to render previously deadly infections into minor inconveniences. Infectious diseases topped the list as the leading cause of mortality for most of human existence. The rise of antibiotics has given us an effective weapon against this invisible enemy.
Evidence suggests that humans have harnessed the power of antibiotics for millennia. For example, traces of the antibiotic tetracycline are present in human skeletal remains[1] from ancient Sudanese Nubia dating back to 350–550 AD.
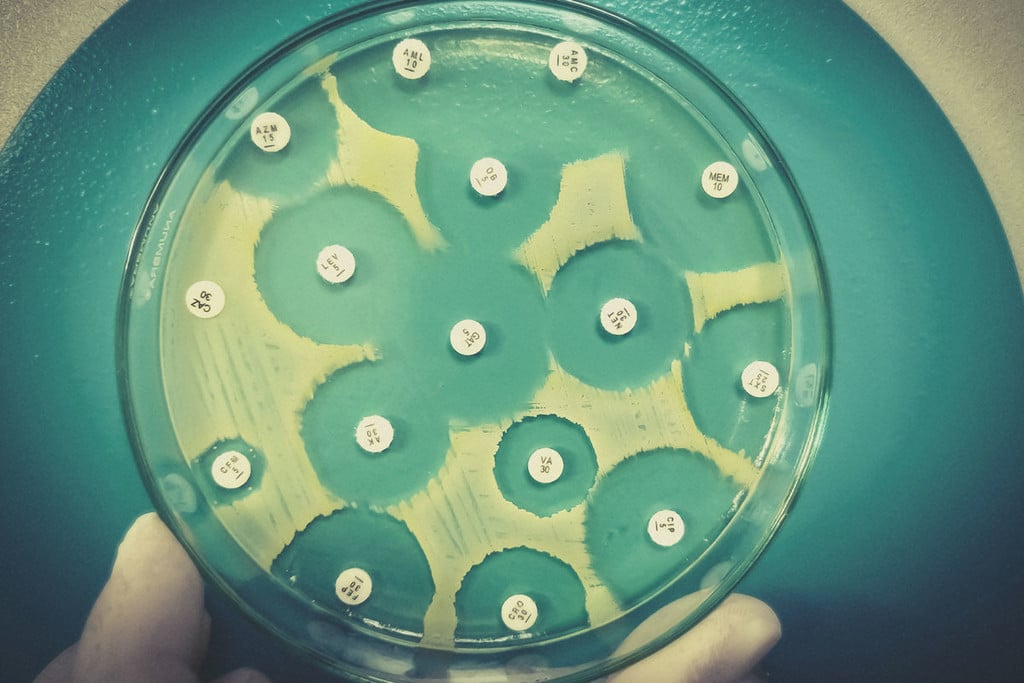
However, most of us associate the emergence of live-saving antibiotics with Alexander Fleming and the start of the “antibiotics era”. Fleming discovered the antibiotic penicillin while studying Staphylococcus bacteria. After leaving a Petri dish filled with the bacteria next to an open window, he returned to find the dish contaminated with mould. However, the new fungal arrival had also successfully killed off the infectious bacteria.
This ground-breaking discovery took place on September 3rd, 1928, and went on to save an estimated 200 million lives[2].
-
How Antibiotics Work
Antibiotics work in two primary ways. They either help to slow cells down (bacteriostatic) or kill them (bactericidal). Bacteriostatic antibiotics stall bacterial cellular activity but don’t cause them to die outright. They essentially put a pause on their ability to multiply, which gives the immune system ample opportunity to wipe out the current infection. These drugs achieve this by interfering with DNA replication, metabolism, and protein production.
In contrast, bactericidal antibiotics directly kill bacteria. They do so by preventing bacteria from forming a cell wall, which quickly leads to their demise. Penicillin antibiotics are bactericidal, including penicillin V for sore throats, and amoxicillin for chest infections.
Antibiotics also differ in the species of bacteria that they target. Some are classed as “broad spectrum” and attack numerous species, including beneficial bacteria that reside in the gut. This can lead to an imbalance within the microbiome and possible digestive issues. In opposition to this mechanism, “narrow-spectrum” antibiotics are more selective in the species they inflict damage against. They only affect between 1–2 types of bacteria, leaving many of our native microbes to live their lives in peace.
-
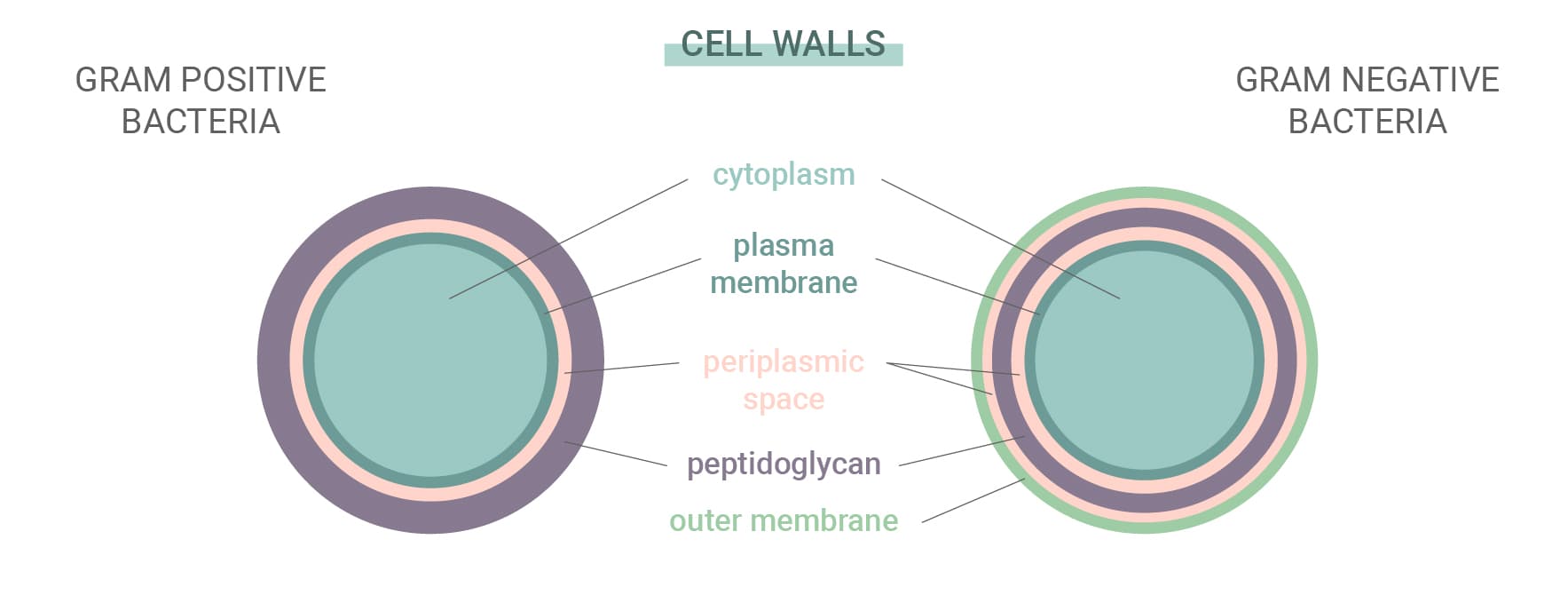
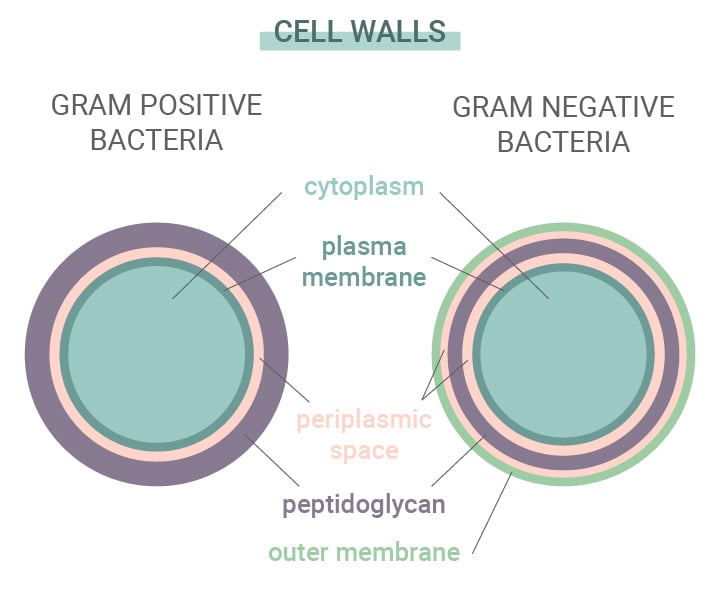
Gram-Positive vs Gram-Negative Bacteria
Some bacteria are more resistant to antibiotics and the antibodies created by our immune system than others. Bacteria autumn into one of two categories: gram-positive and gram-negative. This name derives from a staining test used to identify species of bacteria.
These two types differ based on their cell walls. Gram-positive bacteria have no outer membrane, a complex cell wall, and a thick peptidoglycan (protein and carbohydrate) layer. Gram-negative bacteria, on the other hand, feature an outer lipid membrane and a thin peptidoglycan layer. As gram-negative species have a thicker outer layer, they're often more impervious to antibiotics.
Although the term “antibiotics” literally means “against life”, these drugs only work on a select category of microbes, namely bacteria. Antibiotics cannot protect the body against viruses, for several reasons. First of all, viruses enter host cells to replicate, and bacteriostatic antibiotics do not attack host cells. Second, viruses don’t possess cell walls, which means bactericidal antibiotics have nothing to attack.
The Different Types of Antibiotics
There are several different types of antibiotics available. Each helps to combat different forms of bacterial infections. Although hundreds of antibiotics exist, most of them autumn into the six major groups below:
| Penicillins | This group contains penicillin, amoxicillin, flucloxacillin, and other drugs. Penicillins help to fight off bacteria by preventing them from forming protective cell walls—structures that keep these single-celled organisms together. These drugs are used to treat a wide range of infections, including those of the skin, chest, and urinary tract. |
| Cephalosporins | These broad-spectrum antibiotics are used to combat numerous types of infections, including more serious conditions such as meningitis, pneumonia, and septicaemia. |
| Aminoglycosides | This class of antibiotics is recruited to fight off certain types of gram-negative bacteria. They are sometimes used alongside other forms of antibiotics, and are mostly administered in hospitals due to the risk of severe side effects such as kidney damage. |
| Tetracyclines | Antibiotics belonging to this group, including doxycycline, kill bacteria by disrupting protein synthesis. Although their effectiveness has somewhat waned due to bacterial resistance, they are still used for conditions such as acne. |
| Macrolides | These are prescribed to patients that are allergic to penicillin. Macrolides are also effective at combating lung infections such as pneumonia. |
| Fluoroquinolones | Drugs in this class, such as ciprofloxacin, are rarely prescribed nowadays due to adverse side effects including nausea, vomiting, and sensitivity to sunlight. In the past, physicians prescribed them to fight off respiratory and urinary tract infections. |
| Penicillins |
| This group contains penicillin, amoxicillin, flucloxacillin, and other drugs. Penicillins help to fight off bacteria by preventing them from forming protective cell walls—structures that keep these single-celled organisms together. These drugs are used to treat a wide range of infections, including those of the skin, chest, and urinary tract. |
| Cephalosporins |
| These broad-spectrum antibiotics are used to combat numerous types of infections, including more serious conditions such as meningitis, pneumonia, and septicaemia. |
| Aminoglycosides |
| This class of antibiotics is recruited to fight off certain types of gram-negative bacteria. They are sometimes used alongside other forms of antibiotics, and are mostly administered in hospitals due to the risk of severe side effects such as kidney damage. |
| Tetracyclines |
| Antibiotics belonging to this group, including doxycycline, kill bacteria by disrupting protein synthesis. Although their effectiveness has somewhat waned due to bacterial resistance, they are still used for conditions such as acne. |
| Macrolides |
| These are prescribed to patients that are allergic to penicillin. Macrolides are also effective at combating lung infections such as pneumonia. |
| Fluoroquinolones |
| Drugs in this class, such as ciprofloxacin, are rarely prescribed nowadays due to adverse side effects including nausea, vomiting, and sensitivity to sunlight. In the past, physicians prescribed them to fight off respiratory and urinary tract infections. |
Can You Smoke Weed on Antibiotics?
We all know you should avoid drinking alcohol while taking a course of antibiotics, but what about smoking weed?
Cannabis certainly has a better overall safety profile than booze, but compounds within the plant can interact with an array of other drugs.
Below, you’ll find out how cannabis influences drug metabolism, and if it’s advisable to consume THC or CBD while taking antibiotics.
-
Cannabis Interacts With Other Drugs
Consuming cannabis doesn’t just get you high. Cannabinoids like THC and CBD are capable of impacting the endocannabinoid system throughout the body, resulting in complex and far-reaching biochemical cascades.
Your body breaks down and metabolises everything you consume, including cannabinoids. As a detoxification organ and hub of metabolism, the liver plays an important role in this process. More specifically, the cytochrome P450 family of enzymes is responsible for metabolising several cannabinoids. Members of this enzymatic family are also tasked with metabolising around 90% of drugs[3].
However, due to their interactions with these enzymes, cannabinoids such as THC and CBD inhibit cytochrome P450 drug metabolism[4], which may lead to significant drug-drug interactions. For example, reports have found that cannabis can increase the anticoagulant effect of the drug warfarin by interrupting its metabolism through this mechanism of action. These enzymes are also responsible for metabolising several antibiotics, including erythromycin, which opens up the possibility of adverse reactions.
-
Does THC Interact With Antibiotics?
The research surrounding interactions between THC and antibiotics remains scarce. While THC and some antibiotics both impact the same important liver enzymes, the risk of serious interactions appears relatively low, but this is only anecdotal. Indeed, no in-depth studies have analised the risk, but a few reports exist that document adverse events in people taking both substances simultaneously.
With that said, by altering liver metabolism, THC could increase the odds of experiencing the side effects of antibiotics. Furthermore, smoking anything while experiencing a respiratory infection has the potential to increase the severity[5] of the condition.
Plus, some evidence points to THC as an immunosuppressive agent[6]. We highly recommend letting your doctor know about your cannabis use if you plan on using the herb while taking antibiotics.
-
Does CBD Interact With Antibiotics?
CBD acts as a potent inhibitor of cytochrome P450 enzymes, and therefore may alter the metabolism of certain antibiotics and predispose patients to adverse events and an increased risk of side effects.
As with THC, little to no research exists detailing the level of risk when taking these substances side by side. However, both CBD and antibiotics are taken separately by millions of people every day. People likely often mix the two, and no major reports have detailed severe adverse events. But that does not mean they cannot occur. You should let your doctor know about your CBD use upon receiving an antibiotic prescription, and follow their advice.
-
Is Cannabis the Answer to Antibiotic-Resistant Bacteria?
Science has yet to fully elucidate the implications of taking cannabis and antibiotics at the same time. Intriguingly, however, some researchers are looking to determine if cannabis compounds are themselves antibiotic. As antibiotic-resistant strains of bacteria continue to develop and defy conventional drug options, scientists are testing compounds such as THC and CBD on the microbial battlefield. For example, a study[7] published in the journal Communications Biology set about administering CBD to the “urgent threat” pathogen Neisseria gonorrhoeae to see if it offered any therapeutic potential.
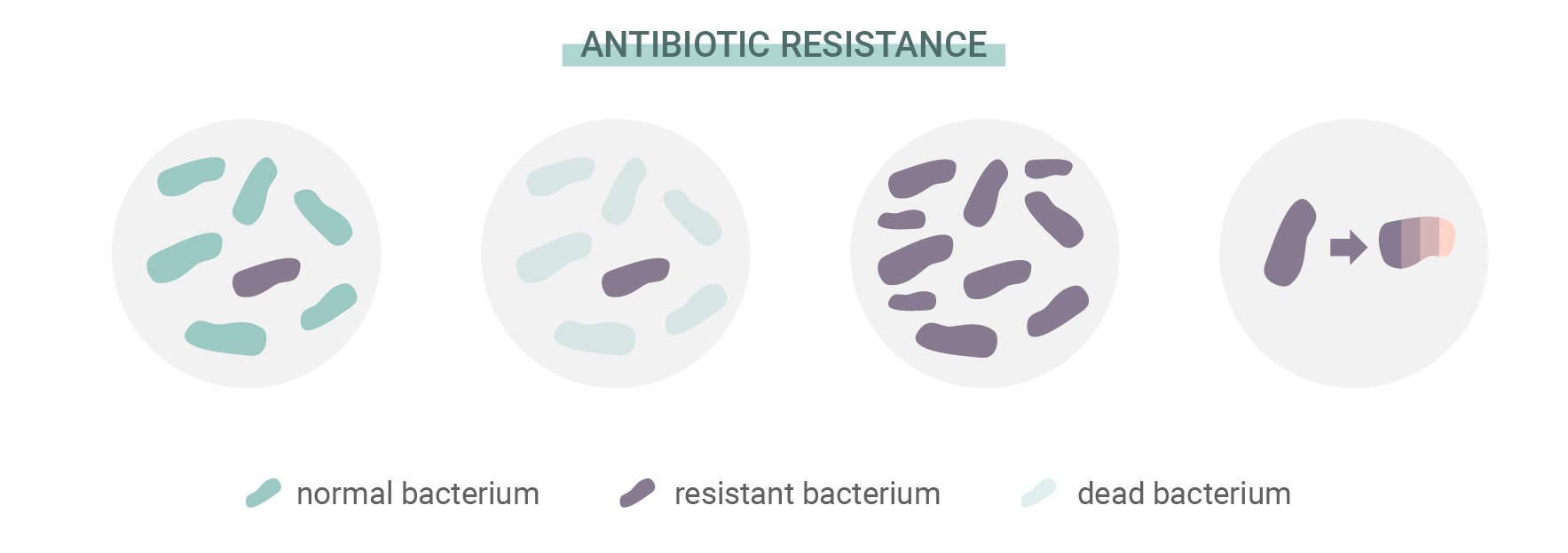
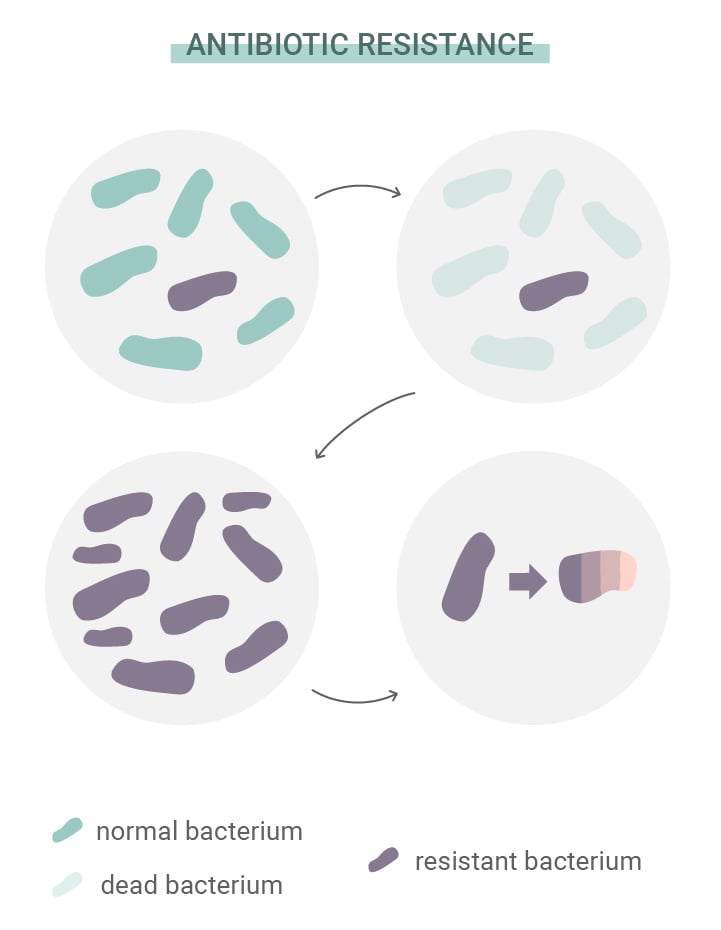
What Is Antibiotic Resistance?
Antibiotics have saved millions of lives, and continue to do so. But bacteria refuse to wait in position like sitting ducks. Like all other life forms on Earth, they possess the ability to adapt to threats, overcome challenges, and ensure their own survival. This trait has enabled some species to develop resistance to antibiotics. The source of this trouble lies in something that guides the development of all life: natural selection.
Just like other organisms, individual bacteria develop random mutations. Some of these are functional, whereas others are completely useless. However, every now and then, one mutation comes along that improves an organism's ability to adapt and survive. Some bacteria develop mutations that make them more resistant to antibiotics than others. As those that are susceptible to antibiotics die off, those that possess the beneficial mutation gain more resources and multiply.
Examples of these successful mutations include the development of Staphylococcus aureus into MRSA (methicillin-resistant Staphylococcus aureus). This form of bacteria has developed resistance to methicillin and penicillin, and manages to keep constructing its cell wall in the face of these antibiotics thanks to a genetic tweak.
-
The Looming Threat of Antibiotic Resistance
The World Health Organisation (WHO) views antibiotic resistance as one of the biggest threats to global health and development. Although antibiotic resistance develops naturally, the WHO points toward the misuse of antibiotics in humans and animals as a factor that aids the process. As a result, infections such as pneumonia, tuberculosis, gonorrhoea, and salmonellosis are becoming harder to treat.
Individuals can help to curb this phenomenon by only taking antibiotics prescribed by health professionals, and by never taking them when they don’t need to. Health professionals can also help to slow the rate of antibiotic resistance by refusing to overprescribe these medicines.
Researchers are also playing their part by hunting down new forms of antibiotics that can tackle mutated strains. But where are they looking? Some are eyeing up cannabis as a potential source of novel antibiotics.


Is Marijuana a Potential Antibiotic?
How can a natural plant possibly stop mutating bacteria in its tracks? Well, first, antibiotics are derived from fungi—a group of naturally occurring organisms. Second, plants have engaged bacteria and other microbes in an evolutionary arms race over millions of years. They have become rather efficient in producing molecules that keep these pathogens at bay.
More specifically, plants largely protect themselves by manufacturing secondary metabolites. These molecules aren’t involved in the growth or development of a plant, but rather serve as chemical weapons. Cannabis plants have quite the arsenal, producing over 100 cannabinoids and 200 terpenes for this purpose.
-
Antibiotic Potential of Cannabinoids and Terpenes
Researchers have explored the antibacterial properties of cannabis extracts and cannabinoids for several decades. The first studies took place in the 1950s. Although the researchers observed bactericidal effects, a lack of knowledge on cannabis phytochemistry at the time prevented them from determining the active constituents.
However, researchers made a breakthrough in 1976 when they discovered the bacteriostatic and bactericidal actions of THC and CBD against gram-positive bacteria. Studies have also tested hemp essential oils against some forms of bacteria.
These preparations include novel cannabinoids, and terpenes such as pinene, limonene, and ocimene. Studies found moderate to good antimicrobial activity in vitro, suggesting that a combination of cannabis constituents might prove beneficial in future human research.
Studies have focused on several different cannabinoids in the search for novel antibiotics. THC, the main psychotropic component of cannabis that causes the “high”, appears to show some promise. Studies are finally exploring its efficacy in greater depth, and findings from a 2008 paper justify further exploration into its effects[8] against MRSA.
What About Other Antibacterial Cannabinoids?
THC often occupies the limelight when it comes to cannabis research. Of course, its psychotropic status is always a hot topic of debate. While some users appreciate these effects, non-psychotropic cannabinoids are more attractive to researchers as they don’t expose patients to such side effects.
| CBD | |||||||
|---|---|---|---|---|---|---|---|
|
CBD, or cannabidiol, produces no high. Instead, users report a clear-headed effect that doesn’t impair cognitive function. CBD has become the focus of hundreds of studies exploring its possible benefits, including its action against antibiotic-resistant bacteria. A 2021 paper titled “The antimicrobial potential of cannabidiol” marked some serious progress[9] in this domain. The data documents CBD’s potential to combat gram-negative “urgent threat” bacteria such as Neisseria gonorrhoeae. |
|||||||
| CBG | |||||||
| Have you ever heard of cannabigerol, aka CBG? Its acidic form, CBGA, is known as the “mother cannabinoid”. This non-psychotropic molecule serves as the chemical precursor to other cannabinoids, including THC and CBD. Researchers have also investigated CBG for its antibiotic potential, with studies comparing it against vancomycin—a medication used to treat numerous types of bacterial infections—in mouse models of MRSA. | |||||||
| CBD | |||||||
|---|---|---|---|---|---|---|---|
|
CBD, or cannabidiol, produces no high. Instead, users report a clear-headed effect that doesn’t impair cognitive function. CBD has become the focus of hundreds of studies exploring its possible benefits, including its action against antibiotic-resistant bacteria. A 2021 paper titled “The antimicrobial potential of cannabidiol” marked some serious progress[9] in this domain. The data documents CBD’s potential to combat gram-negative “urgent threat” bacteria such as Neisseria gonorrhoeae. |
|||||||
| CBG | |||||||
| Have you ever heard of cannabigerol, aka CBG? Its acidic form, CBGA, is known as the “mother cannabinoid”. This non-psychotropic molecule serves as the chemical precursor to other cannabinoids, including THC and CBD. Researchers have also investigated CBG for its antibiotic potential, with studies comparing it against vancomycin—a medication used to treat numerous types of bacterial infections—in mouse models of MRSA. | |||||||
The Future for Cannabis as an Antibiotic
So, can we expect to see cannabis-based antibiotics behind pharmacy counters any time soon? Not just yet. Researchers have tested cannabinoids against worrying emerging strains of bacteria, but the studies remain preclinical.
As science continues to pitch THC, CBD, and other molecules against Petri dish pathogens, we hope to also see more research emerge in the area of drug interactions between cannabis and antibiotics. New findings in this area will help patients and physicians alike in terms of continuing or discontinuing cannabis use when treating infections with antibiotics.
Medical DisclaimerInformation listed, referenced or linked to on this website is for general educational purposes only and does not provide professional medical or legal advice.
Royal Queen Seeds does not condone, advocate or promote licit or illicit drug use. Royal Queen Seeds Cannot be held responsible for material from references on our pages or on pages to which we provide links, which condone, advocate or promote licit or illicit drug use or illegal activities.
Please consult your Doctor/Health care Practitioner before using any products/methods listed, referenced or linked to on this website.
- A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future https://www.ncbi.nlm.nih.gov
- One discovery that changed the world | Florey 120 Anniversary | University of Adelaide https://health.adelaide.edu.au
- The Effect of Cytochrome P450 Metabolism on Drug Response, Interactions, and Adverse Effects https://www.aafp.org
- Cannabinoid Interactions with Cytochrome P450 Drug Metabolism https://pubmed.ncbi.nlm.nih.gov
- Smoking in acute respiratory infections https://www.cebm.net
- How cannabis suppresses immune functions https://www.sciencedaily.com
- The antimicrobial potential of cannabidiol https://www.nature.com
- Antibacterial cannabinoids from Cannabis sativa: a structure-activity study - PubMed https://pubmed.ncbi.nlm.nih.gov
- The antimicrobial potential of cannabidiol | Communications Biology https://www.nature.com