.

The Relationship Between Cannabis and Diabetes
Cannabis and diabetes. You don't see those two words placed together very often. However, that seems poised to change. Research has started to explore how cannabis constituents affect markers of diabetes. Studies have also sought to discover the relationship between cannabis use and the risk of developing diabetes. So, what's the verdict?
Contents:
What do you need to know when it comes to marijuana and diabetes? Does weed lower blood sugar? Can diabetics smoke weed? Are sugar-free edibles a better option? We’re going to dive into these questions and more below. First, we’ll look at diabetes as a whole, and how it affects the body. Then, we’ll examine the existing research on how cannabis might impact the condition.
What Is Diabetes?
Without fuel, your car wouldn’t make it out of the driveway, and without carbohydrates, your body wouldn’t make it out of bed in the morning (the body can run quite efficiently off of fat and ketones, but that’s a whole different story). Whenever we consume carb-containing foods, our body does a good job of breaking it down into simple glucose molecules and ferrying it off into our cells as a vital energy source.
Our body relies on the pancreas—an organ situated just behind the stomach—to carry out this process. This gland secretes the hormone insulin in response to glucose. This molecule works like a “key” to cells; it takes glucose out of the bloodstream and moves it into various cells throughout the body.
Under normal circumstances, this process keeps our cells energised and our blood sugar levels regulated. However, things go awry in the context of diabetes—a physiological condition in which the body doesn’t make enough insulin, or can’t use the insulin that it does produce correctly. As a result, high levels of glucose become stuck in the bloodstream. This results in short-term symptoms, such as frequent urination and increased thirst, but over time, diabetes can contribute to more serious health conditions including heart disease and kidney damage.
Over 500 million adults[1] around the world live with diabetes, and projections estimate that this figure will reach almost 800 million by 2045; the condition poses a significant global health issue. There are two types of diabetes that affect this population. Learn about their differences below.
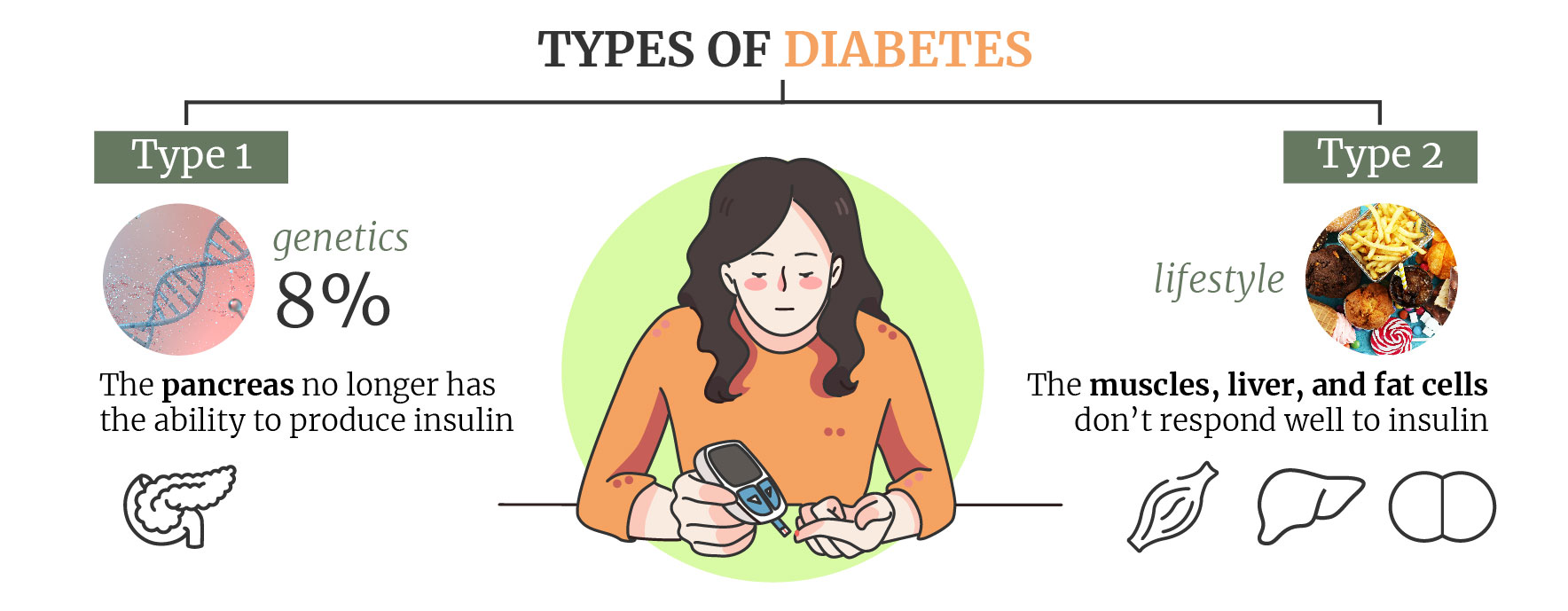
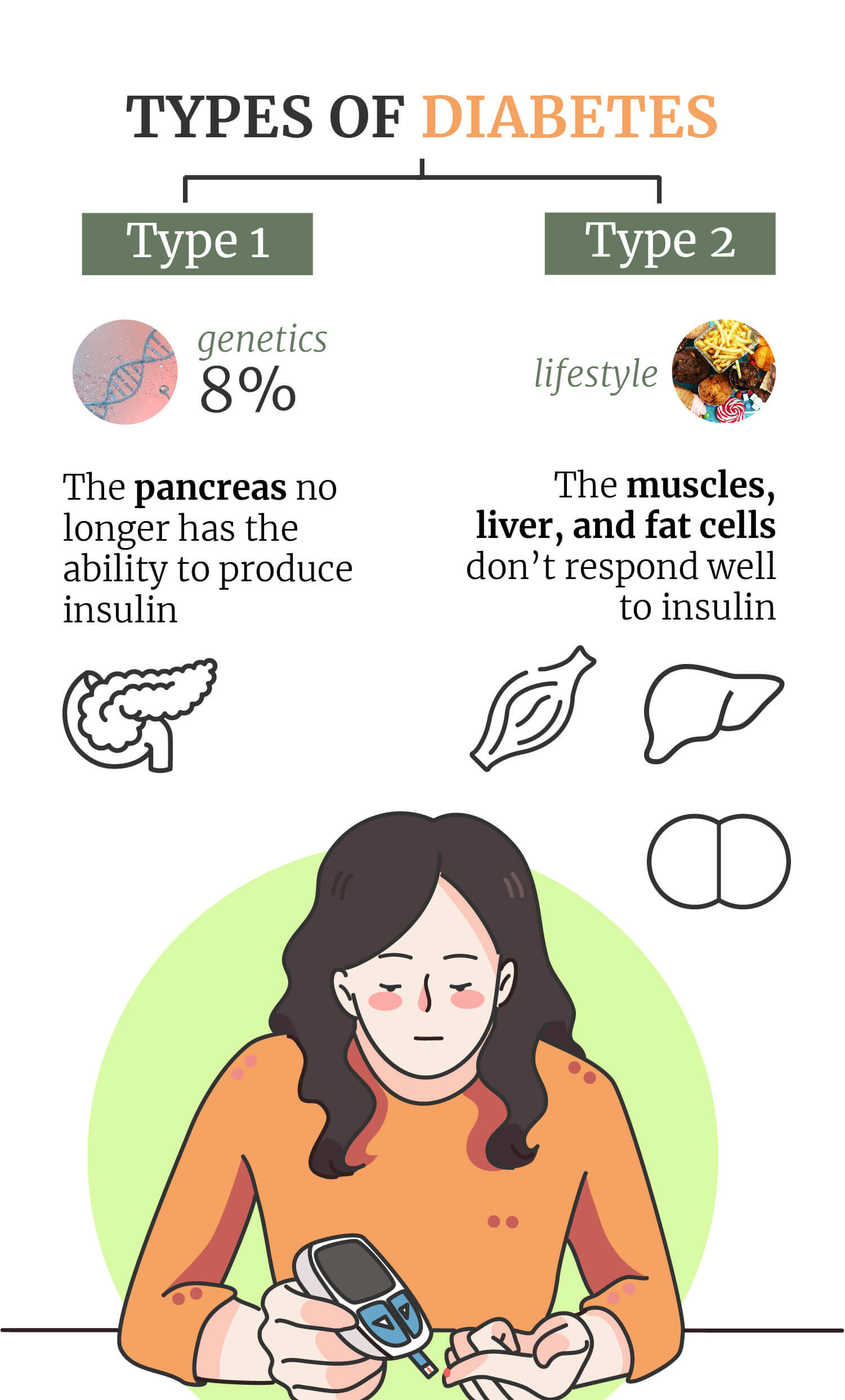
Type 1 Diabetes
Type 1 diabetes has its roots in a genetic condition rather than lifestyle factors. For this reason, type 1 usually shows up earlier in life. As a type of autoimmune disease, it’s caused by components of the immune system attacking the insulin-producing cells in the pancreas.
Following this self-inflicted damage, the pancreas no longer has the ability to produce insulin and cannot respond appropriately to glucose in the bloodstream. Scientists still don’t completely understand what causes the body to commit this physiological assault on itself, and no cure currently exists. People with type 1 diabetes take insulin to help control their blood sugar levels.
Type 2 Diabetes
Whereas only 8% of diabetes patients are affected by type 1, type 2 affects the vast majority[2]. Although genetic factors can increase the risk of developing type 2 diabetes, lifestyle factors such as obesity can drastically increase the odds; adipose (fat) tissue causes cells of the body to become less sensitive to insulin.
This type of diabetes starts with a state known as insulin resistance. Here, the muscles, liver, and fat cells don’t respond well to insulin, meaning high levels of glucose remain in the bloodstream. This causes the pancreas to ramp up insulin production in an attempt to store the excess glucose. Over time, the increased activity exhausts the pancreas, and it struggles to make the critical hormone. While no cure exists, medication, exercise, diet, and insulin are used to manage this form of the condition.
How Diabetes Affects the Body
Diabetes affects the body in many different ways. The symptoms can be divided into acute (short-term) and chronic (long-term). Let’s look at the acute symptoms of diabetes first:
| Increased thirst | Extreme hunger |
| Frequent urination | Unexplained weight loss |
| Irritability | Fatigue |
| Blurred vision |
| Increased thirst | Extreme hunger |
| Frequent urination | Unexplained weight loss |
| Irritability | Fatigue |
| Blurred vision |
Over time, diabetes can lead to chronic symptoms and complications such as:
| Heart disease | Nerve damage |
| Kidney damage | Eye damage |
| Limp damage leading to amputation | Skin issues |
| Hearing problems | Alzheimer’s disease |
| Depression |
| Heart disease | Nerve damage |
| Kidney damage | Eye damage |
| Limp damage leading to amputation | Skin issues |
| Hearing problems | Alzheimer’s disease |
| Depression |
Pros of Outdoor Hydroponics
So, should you grow hydro marijuana outdoors? Find out why it might work for you.
Cannabis and Diabetes
In recent years, cannabis has started to emerge from its status as a vilified substance and become a subject of extreme interest to researchers in the medical field. Several decades ago, while studying the components of this fascinating herb, researchers discovered the endocannabinoid system (ECS). In doing so, they partially unveiled the specific pathway through which certain constituents of the plant are able to influence human physiology.
Currently, researchers are testing cannabinoids (molecules that interface with the ECS) against a host of different diseases, including diabetes. Before we look at some research on this matter, we need to get to grips with the ECS. Knowing a bit more about this system will help you better understand the relationship between marijuana and diabetes.
The Role of the Endocannabinoid System in Diabetes
Known as the “universal regulator” of the human body, the ECS helps to keep all of our physiological systems in balance. This system governs neurochemical firing in the brain, oversees bone growth and breakdown, assists energy balance, and even resides in the skin to ensure the adequate turnover of cells. The ECS consists of a series of receptors, signalling molecules that bind to these receptors, and enzymes that create and destroy the signalling molecules. Wherever you look in the body, you’ll find the ECS acting as somewhat of a traffic controller, ensuring things are running smoothly.
However, the ECS doesn’t always operate perfectly. Various factors, such as genetics and diet, can cause this system to malfunction. Because it plays such a key role in mediating other systems and processes, things can get pretty serious when it falters. An emerging theory known as clinical endocannabinoid deficiency posits that a dysfunction within the ECS can lead to conditions such as migraine, irritable bowel syndrome, and fibromyalgia.
It appears that the ECS also plays a role in governing processes affecting the pathophysiology of diabetes. It’s implicated[3] in the regulation of body weight, food intake, hyperglycaemia (high blood sugar), insulin resistance, and dyslipidemia (the imbalance of lipids such as cholesterol).
The involvement of the ECS in these processes makes it a potential target in the treatment and prevention of diabetes. It just so happens that cannabinoids found in cannabis (phytocannabinoids) share a similar structure to those found in our body (endocannabinoids), meaning they could potentially be used to target this system.
With that in mind, let’s take a look at what the research says about cannabis, cannabinoids, and diabetes.
Association Between Cannabis Use and Diabetes
Can cannabis help to manage or even prevent diabetes? We don’t have the answers to those critical questions yet, due to a lack of controlled human trials. However, epidemiological data has helped to paint a picture of what cannabis might do for people living with diabetes.
A 2013 study[4] published in The American Journal of Medicine examines how regular cannabis use affects some of the health variables associated with diabetic control. Based on a survey of 4,657 patients, self-reported data shows that cannabis users had significantly lower fasting insulin levels and a lower likelihood of insulin resistance compared to non-users. The researchers also noted lower glucose levels and lower waist circumference in past and current users.
The same study highlights that previous studies have also found lower rates of obesity and diabetes in cannabis users, which suggests cannabinoids could manipulate metabolic processes in a favourable way.
While controlled human trials haven’t confirmed these findings, preclinical studies have set out to determine if cannabis constituents could help to manage diabetes symptoms and prevent the condition in the first place. The cannabis plant contains over 100 cannabinoids, and two among them have come to the fore in diabetes research.
As a homologue of THC, tetrahydrocannabivarin (THCV) shares a similar molecular structure to the primary psychotropic cannabinoid. However, the presence of a 3-carbon side chain (instead of the 5-carbon side chain attached to THC) means THCV produces different effects in the body. THCV is a selective agonist of CB1 receptors of the ECS, but only produces a psychoactive effect[5] at higher doses. Early animal research[6] centred around the cannabinoid has set out to see how THCV impacts appetite, energy metabolism, weight loss, and the management of type 2 diabetes.
CBD and Diabetes
CBD also ranks as one of the most promising cannabinoids when it comes to diabetes research. Unlike THC and THCV, CBD does not produce a psychotropic effect at any dose, which makes it more suitable for a larger number of patients.
Inflammation plays an important role in diabetes, and future research aims to investigate these pathways[7] more thoroughly. A battery of preclinical studies have thus far pitched the cannabinoid against models of diabetes in order to assess if it lowers incidence[8], offers neuroprotective effects[9], or helps to stave off[10] autoimmunity associated with type 1 diabetes. A 2015 study [11] performed at the Hebrew University of Jerusalem assessed the anti-inflammatory potential of CBD. Their findings suggest that future research should strive to see if and how CBD impacts diabetes and metabolism through its effects on the immune response.
Risks of Cannabis Use in People With Diabetes
Can diabetics smoke weed? Early epidemiological findings paint a positive picture, but there are some risks involved. To start, anyone who uses cannabis knows how it kindles the appetite and often drives people to seek out sugar-rich foods. Plus, not all findings have churned out optimistic results. A 2020 review[12] of available data associated cannabis use with poor self-management behaviours in people with type 1 diabetes, and an increased risk of peripheral arterial occlusion, heart attack, and kidney diseases in those with type 2 diabetes.
In regard to CBD, case reports have shown that the cannabinoid doesn’t appear to cause harm or worsen diabetes control. However, taking CBD alongside the diabetes drug metformin could increase the risk of stomach upset[13].
Edibles for Diabetics
What about edibles for diabetes? While sugar-free edibles aren’t necessarily aimed at people living with diabetes, they’re more likely to appeal to such individuals. When snacking, many diabetic patients opt for foods with a low glycaemic index (GI) to avoid a surge in blood glucose. Lucky for them, a range of sugar-free edibles are available in legal regions, including crackers, chocolate, candy, coffee, and tea.
The Future of Cannabis and Diabetes
Existing preclinical evidence shows early promise. However, tightly controlled human trials are needed to confirm just how cannabis affects insulin, blood glucose, appetite, body weight, and other biological markers associated with diabetes.
Moreover, researchers have barely scratched the surface when it comes to testing cannabinoid constituents against models of the condition. Because of this, anybody living with diabetes that wants to continue to use cannabis, or incorporate it into their life, should consult their medical professional for advice on the safest way to do so.
- Diabetes https://www.who.int
- Efficacy and Safety of Cannabidiol and Tetrahydrocannabivarin on Glycemic and Lipid Parameters in Patients With Type 2 Diabetes http://care.diabetesjournals.org
- The Role of Cannabis and Cannabinoids in Diabetes https://www.researchgate.net
- Novel Study Reports Marijuana Users Have Better Blood Sugar Control https://realmofcaring.org
- Cannabinoid Pharmacology https://www.sciencedirect.com
- Δ9-Tetrahydrocannabivarin (THCV): a commentary on potential therapeutic benefit for the management of obesity and diabetes | Journal of Cannabis Research | Full Text https://jcannabisresearch.biomedcentral.com
- The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives - PMC https://www.ncbi.nlm.nih.gov
- Cannabidiol lowers incidence of diabetes in non-obese diabetic mice https://www.tandfonline.com
- Neuroprotective and Blood-Retinal Barrier-Preserving Effects of Cannabidiol in Experimental Diabetes https://www.sciencedirect.com
- Cannabidiol arrests onset of autoimmune diabetes in NOD mice https://www.sciencedirect.com
- CBD compound in cannabis could treat diabetes, researchers suggest - Diabetes https://www.diabetes.co.uk
- The effects of recreational cannabis use on glycemic outcomes and self-management behaviours in people with type 1 and type 2 diabetes: a rapid review - PMC https://www.ncbi.nlm.nih.gov
- CBD and other medications: Proceed with caution - Harvard Health https://www.health.harvard.edu