.

Cannabis and Glaucoma: What You Need to Know
Researchers are still grappling to find the cause of glaucoma. The eye condition eventually leads to vision loss due to raising pressure within the eye and damaging the optic nerve. No cures currently exist and conventional treatments only slow the progression. Researchers are now looking to cannabis as a potential reservoir of therapeutics.
Contents:
Glaucoma—this pathology of the eyes results in a battery of symptoms, including gradual vision loss. Researchers aren’t completely sure what causes the condition, and conventional treatments only serve to slow the progression down. Now, researchers are probing cannabis in search of phytochemicals that might help.
What Is Glaucoma?
Glaucoma is caused by a group of diseases that result in degeneration of the optic nerve—a branch of the central nervous system that transmits electrical impulses from the eyes to the brain. Glaucoma ranks as the second leading cause of blindness across the world and can affect individuals from all age groups, although people over 60 are at a higher risk of developing the condition. Currently, over 70 million[1] people worldwide are thought to have glaucoma. Because the symptoms can remain elusive, only 10–50% of this population know about their condition.
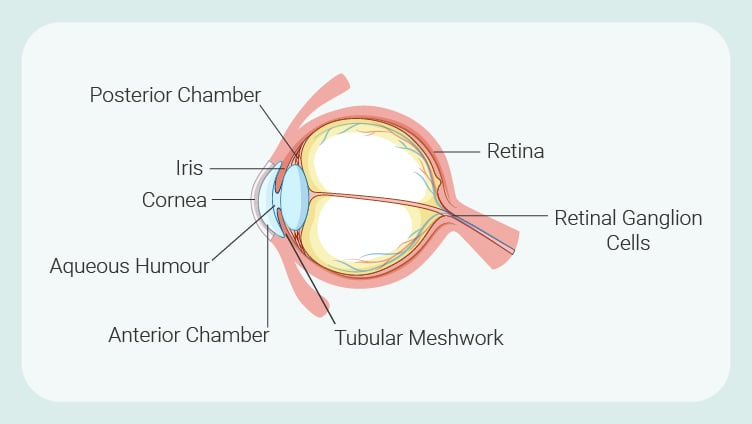
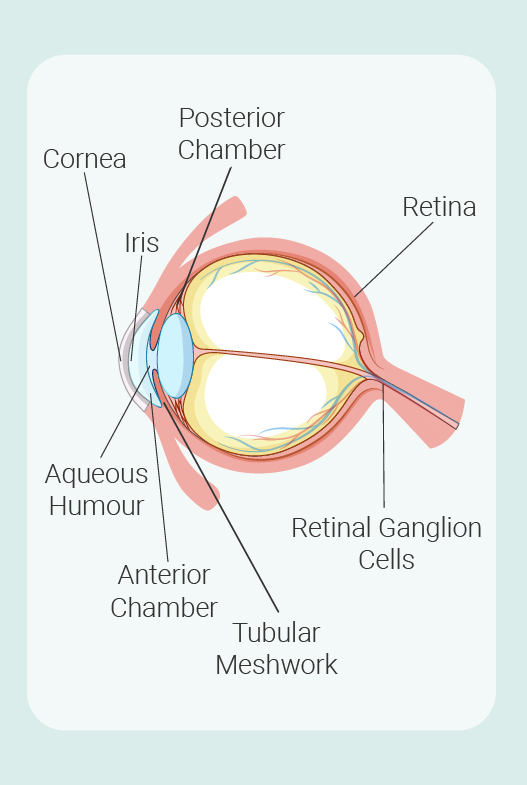
To fully understand glaucoma, it helps to know about the key components and systems of the eyes that are implicated in the condition. Learn more about them below:
|
Retina: Located close to the optic nerve at the back of the eye, this layer of tissue features photoreceptors in the form of cones and rods that convert light into electrical signals. |
Retinal ganglion cells: These neurons make up the optic nerve. Collectively, they transmit visual information from the retina and deliver it to specific regions of the brain. |
Aqueous humour: This clear fluid contains small quantities of protein and glucose and higher concentrations of lactic acid and ascorbic acid (vitamin C). First produced in a muscular tissue known as the ciliary body, aqueous humour flows through chambers in the eye where it distributes these nutrients alongside oxygen. |
Trabecular meshwork: Located towards the front of the eye, this porous tissue facilitates the drainage of aqueous humour from the eyes and, in doing so, helps to regulate pressure within the eye (also known as intraocular pressure). |
|
Iris: The coloured part of the eye (some of us have green iris, some blue or brown or other colours). This structure in the eye helps to regulate the amount of light that gets through by opening and closing the pupil based on light intensity. |
Cornea: As the outermost lens of the eyes, the cornea plays a protective role. It also refracts light and focuses light onto the retina. |
Posterior chamber: Following production in the ciliary body, aqueous humour flows through this open space between the pupil and the iris. |
Anterior chamber: After passing through the pupil, aqueous humour flows through this space, between the iris and the cornea, and out towards the trabecular meshwork. |
|
Retina: Located close to the optic nerve at the back of the eye, this layer of tissue features photoreceptors in the form of cones and rods that convert light into electrical signals. |
Retinal ganglion cells: These neurons make up the optic nerve. Collectively, they transmit visual information from the retina and deliver it to specific regions of the brain. |
|
Aqueous humour: This clear fluid contains small quantities of protein and glucose and higher concentrations of lactic acid and ascorbic acid (vitamin C). First produced in a muscular tissue known as the ciliary body, aqueous humour flows through chambers in the eye where it distributes these nutrients alongside oxygen. |
Trabecular meshwork: Located towards the front of the eye, this porous tissue facilitates the drainage of aqueous humour from the eyes and, in doing so, helps to regulate pressure within the eye (also known as intraocular pressure). |
|
Iris: The coloured part of the eye (some of us have green iris, some blue or brown or other colours). This structure in the eye helps to regulate the amount of light that gets through by opening and closing the pupil based on light intensity. |
Cornea: As the outermost lens of the eyes, the cornea plays a protective role. It also refracts light and focuses light onto the retina. |
|
Posterior chamber: Following production in the ciliary body, aqueous humour flows through this open space between the pupil and the iris. |
Anterior chamber: After passing through the pupil, aqueous humour flows through this space, between the iris and the cornea, and out towards the trabecular meshwork. |
Now that you’re familiar with some key components of eye anatomy, let’s take a look at two of the major types of glaucoma and how they affect vision.
How Glaucoma Affects Vision
So, how exactly does glaucoma affect vision? Well, it has a lot to do with intraocular pressure (IOP) and resulting ocular nerve damage due to obstructions in aqueous humour flow. Below, we’re going to look at two of the primary forms of glaucoma and how they result in nerve damage and eventual vision loss. The exact cause of both types of glaucoma remains unknown. However, researchers have found that the buildup of IOP occurs due to the narrowing of either the anterior or posterior chambers.
- Primary open-angle glaucoma: This type of glaucoma results in the collapse of the iris into the posterior chamber. This reduces the flow of aqueous humour through the pupil, causing a backflow that leads to an increase in IOP. Part of the iris also collapses forward, blocking aqueous humour flow from reaching the trabecular meshwork. Subsequently, this causes mechanical stress on structures towards the back of the eye, resulting in compression, deformation, and disrupted nervous system firing. This blockage also prevents the delivery of trophic factors to the retinal ganglion cells—substances that support nerve cell health—and results in neurodegeneration. Interestingly, some patients with high IOP don’t develop other symptoms of glaucoma.
- Primary closed-angle glaucoma: This form of glaucoma occurs due to increased resistance of the trabecular meshwork draining aqueous humour from the anterior chamber. While aqueous humour manages to flow unobstructed through the pupil, the outflow through the trabecular meshwork is reduced, leading to an increase in IOP.
Symptoms of Glaucoma
These contributing mechanisms of glaucoma result in an array of symptoms, including:
|
Severe eye pain Nausea and vomiting Headache Red eyes |
Tender eyes Seeing rings around lights Blurred vision Vision loss |
Conventional Treatments and Risk Factors
Various risk factors contribute to the odds of somebody developing glaucoma. These include:
- Being over age 60
- Being of African, Asian, or Hispanic descent
- Family history of glaucoma
- Medical conditions such as diabetes, heart disease, and high blood pressure
- Having thin corneas
- Eye injuries
While no cure currently exists, several conventional treatment options are available for glaucoma patients aimed at producing an IOP lowering effect and slowing the progression of vision loss. These include:
- Eye drop medications including prostaglandins, beta-blockers, and alpha-adrenergic agonists
- Oral medications such as carbonic anhydrase inhibitors
- Surgery and therapies including laser therapy, filtering surgery, drainage tubes, and minimally invasive glaucoma surgery (MIGS)

Cannabis and Glaucoma
So, where does cannabis come into all of this? Researchers are currently exploring if compounds found within the cannabis plant can reduce IOP and protect the optic nerve from damage. To understand how the herb might produce these effects, we need to look at the endocannabinoid system (ECS) and how this regulatory network operates in the eye. After covering the role of the ECS, we’ll go over the available research regarding several cannabis compounds and glaucoma.
Weed for Glaucoma: The Endocannabinoid System of the Eye
Have you heard of the ECS? Researchers discovered the first components of this system back in 1988 and they’re still discovering new aspects of it today. To put it simply, the ECS serves as the universal regulator of the human body. It shows up in the brain, skin, immune system, metabolic processes, bones, connective tissue, and muscle. Across the body, it works to maintain biological balance or homeostasis. It keeps things running smoothly and, in doing so, keeps us alive and well.
The ECS comprises two primary receptors known as CB1 and CB2. It also features two key signalling molecules (anandamide and 2-AG), known as endocannabinoids, that bind to these receptors to make the necessary changes within target cells. The third key component, a group of specialised enzymes, build and breakdown these endocannabinoids. However, these parts only make up the classical ECS. Researchers have since expanded this system into the endocannabinoidome (eCBome) which features many more receptors, signalling molecules, and enzymes.
Now comes the astonishing part. The cannabis plant produces a set of chemicals known as phytocannabinoids. Among this group are THC, CBD, CBC, CBG, and others (although the plant makes their acidic precursors; these compounds are mostly produced post-harvest when exposed to heat). Interestingly, several of these compounds, including THC, share a common molecular structure with our endocannabinoids. This enables them to latch on to the same receptors and influence our physiology. Other phytocannabinoids, such as CBD, bind to other eCBome sites and also influence ECS enzyme activity. All in all, this means molecules from the cannabis plant have the ability to influence our universal regulator and all of the systems that the ECS holds sway over, including the eyes.
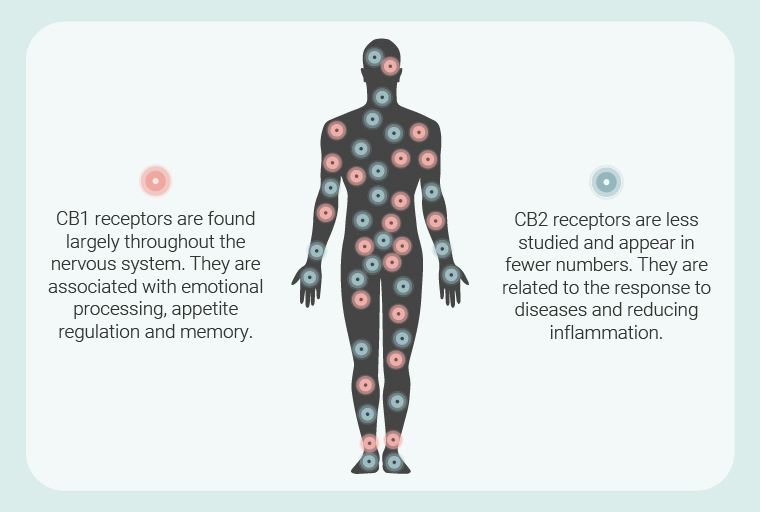
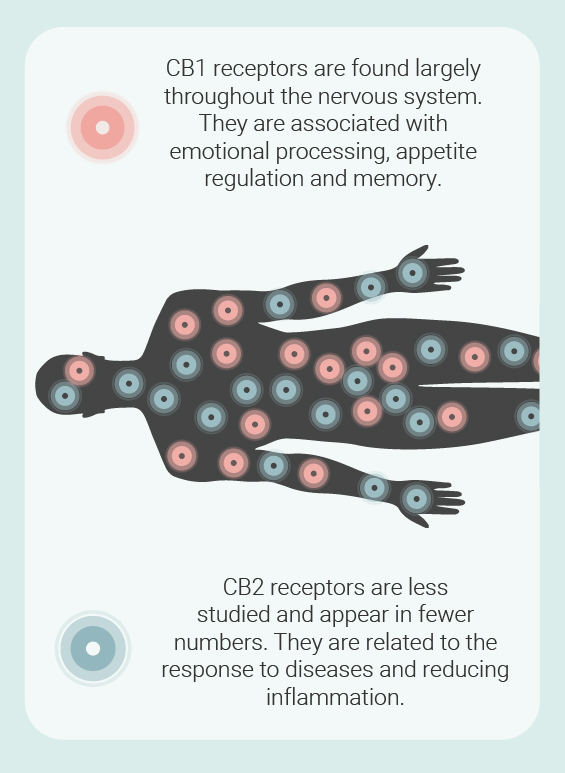
The ECS appears in most ocular tissues, meaning phytocannabinoids can target the homeostatic apparatus within the eyes. Both anandamide and 2-AG are found throughout the tissues of the eyes[2]; though they don’t show up in the lens. But these signalling molecules aren’t alone. They’re accompanied by CB1 receptors that are expressed in the ciliary body[3] (remember this aqueous humour-producing structure from earlier?) and retina, among other locations. Research also suggests that CB2 receptors show up in the retina and front region of the eye. Other eCBome receptors are also present, including transient receptor potential vanilloid 1 (TRPV-1), G protein-coupled receptor 18 (GPR18), and possibly GPR55—various phytocannabinoids and endocannabinoids bind to these sites. Finally, animal studies have also identified ECS enzymes in eye tissues.
Because the ECS keeps physiological systems in balance, things can quickly go south when it malfunctions. The theory of clinical endocannabinoid deficiency has linked reduced levels of circulating endocannabinoids with pathologies such as migraine, irritable bowel syndrome, and fibromyalgia. However, elevated ECS signalling may also drive states such as obesity[4]. The term “endocannabinoid tone” describes a person’s circulating levels of these signalling molecules. An ideal sweet spot could exist to keep things running smoothly, and this level of tone probably varies between individuals.
Limited research has found that alterations in ECS signalling may contribute to glaucoma and other eye conditions. Levels of anandamide and 2-AG appear elevated in cases of diabetic retinopathy, and anandamide levels above normal levels in the ciliary body, cornea, and retina in age-related macular degeneration. Only one study has looked at endocannabinoid levels regarding glaucoma. This research showed reduced levels of 2-AG and PEA[5] (another endocannabinoid) in the ciliary body. PEA also lacked in the post-mortem eyes of glaucoma patients. Interestingly, THC somewhat mimics anandamide in the body, and CBD acts as the phytocannabinoid equivalent of PEA[6], suggesting these two cannabinoids could step in as exogenous signalling molecules.
So, we know the ECS likely plays a role in the pathology of glaucoma. However, future studies are required to identify how critical the role is, and if cannabinoids sourced from outside the body can help by targeting the receptor sites left inactivated by low levels of endocannabinoids. But what about marijuana for glaucoma? Let’s take a look at the research that has tested several plant-derived cannabinoids in models of glaucoma.
THC and Glaucoma
Every cannabis user knows about THC. Known to science as Δ-9-tetrahydrocannabinol, this molecule underpins the cannabis high through activation of the CB1 receptor in the central nervous system. As a meroterpene, THC is part terpene and part phenol. As well as binding to CB1, this constituent also activates the CB2 receptor.
A review[7] published in the journal Neural Plasticity analised previous research to determine if the ECS could serve as a therapeutic target in cases of glaucoma. Citing a collection of rodent, rabbit, and primate studies, as well as one human study, the authors state that cannabinoids modulate IOP. Ongoing human studies are testing both THC and synthetic cannabinoids in cases of glaucoma to see if these chemicals are able to reduce IOP and the accompanying symptoms of glaucoma.
However, cannabinoids might help beyond simply shifting IOP. Despite drugs that lower IOP, glaucoma patients still experience vision loss. The review points out studies that are seeking to determine the neuroprotective effects of cannabinoids that could, in theory, help to shield the optic nerve. Various studies are looking into the neuroprotective effects of THC, including efforts to pitch the cannabinoid against models of Parkinson’s disease.
CBD and Glaucoma
CBD has risen to fame within the cannabis space in recent years. Occurring as the second-most abundant cannabinoid in the majority of modern varieties, this molecule produces no psychotropic effect. However, breeders have developed strains that contain high levels of CBD and next to no THC. CBD has a low affinity for both the CB1 and CBD 2 receptors. However, it manages to influence ECS enzyme activity and also binds to TRPV-1.
But where does CBD fit into the picture when discussing marijuana for glaucoma? The research above suggests that lowered anandamide levels might play a role in the condition. Interestingly, CBD might help to elevate the levels of this endocannabinoid by temporarily inhibiting the enzymes[8] that break it down.
Despite this promising effect, some research shows less promising outcomes. Several studies show that CBD might raise intraocular pressure[9] and therefore pose a risk for glaucoma patients. However, the evidence remains inconclusive. Ongoing studies are also pitching CBD against models of pain and nausea—two symptoms of glaucoma.
Marijuana for Glaucoma: What About CBG?
Cannabigerol, or CBG comes about following the decarboxylation of CBGA. Many know CBG as the “mother cannabinoid”. However, it’s CBGA that serves as the chemical precursor to other major cannabinoid acids, including THCA and CBGA. Ongoing studies[10] are exploring the potential of CBG against a range of conditions, including neurological disorders and inflammatory bowel disease. The cannabinoid binds to both the CB1 and CB2 receptors[11].
Not much research has put CBG up against models of glaucoma. A study[12] published in 2008 investigated the cannabinoid to see if it influenced intraocular pressure. However, human trials are needed to determine if CBG can help people experiencing the condition.
Cannabis and Glaucoma: How Patients Experiment
There are myriad ways to use cannabis. Whereas smoking cannabis proves one of the most popular ways to use the herb, it involves combusting plant material and generating toxic byproducts. Moreover, an association exists between smoking and glaucoma[13]. So, let’s look at a few other options:
- Vaping: Vaporisation uses lower temperatures to volatilise cannabinoids and terpenes. While it still poses some health risks, it exposes users to fewer byproducts than smoking. Overall, vaping offers a fast-acting effect and easy dose modulation.
- Oral: Consuming cannabinoids infused into food and beverages, or administering oral oils, sends these molecules through the digestive tract. Using this way of administration, these chemicals generally have poor bioavailability. However, THC-infused edibles are renowned for their potency, as the liver converts THC into the more potent 11-hydroxy-THC. You should calculate your edible dosage and go low and slow to avoid an unpleasant experience when using ingestible cannabis products.
- Sublingual: This form of administration involves placing extracts or oils under the tongue to allow cannabinoids to diffuse into the bloodstream. This method bypasses the poor bioavailability of oral cannabis without having to inhale smoke or vapour.
Marijuana and Glaucoma: A Complex Relationship
Does cannabis help glaucoma? We can’t say. Not yet. Further human trials featuring large sample sizes are required to find out if the herb offers a potential solution. So far, THC and CBG have shown some promise in early research. Conversely, CBD appears to raise intraocular pressure. Further studies are required to see if this molecule can offer relief or worsen outcomes. If you’re thinking of trying marijuana for glaucoma, we suggest talking to your medical professional to rule out any drug interactions or health complications.
- The Pathophysiology and Treatment of Glaucoma - PMC https://www.ncbi.nlm.nih.gov
- The Endocannabinoid System as a Therapeutic Target in Glaucoma - PMC https://www.ncbi.nlm.nih.gov
- The Endocannabinoid System as a Therapeutic Target in Glaucoma - PMC https://www.ncbi.nlm.nih.gov
- Endocannabinoid system and its implications for obesity and cardiometabolic risk | European Heart Journal Supplements | Oxford Academic https://academic.oup.com
- The Endocannabinoid System as a Therapeutic Target in Glaucoma - PMC https://www.ncbi.nlm.nih.gov
- Endocannabinoid system mediates the association between gut-microbial diversity and anhedonia/amotivation in a general population cohort | Molecular Psychiatry https://www.nature.com
- https://www.hindawi.com/journals/np/2016/9364091/
- https://bpspubs.onlinelibrary.wiley.com/doi/10.1002/prp2.682
- https://www.tandfonline.com/doi/full/10.1080/17469899.2019.1698947
- The Pharmacological Case for Cannabigerol | Journal of Pharmacology and Experimental Therapeutics https://jpet.aspetjournals.org
- https://www.sciencedirect.com/topics/neuroscience/cannabigerol
- [Possibilities of applying cannabinoids' in the treatment of glaucoma] - PubMed https://pubmed.ncbi.nlm.nih.gov
- Smoking and incidence of glaucoma - PMC https://www.ncbi.nlm.nih.gov





































