.

Cannabis and Melanoma: What We Know So Far
Molecules within cannabis impact the endocannabinoid system—the universal regulator that oversees every system in the body. Researchers are continuing to explore this network, which also occurs in the skin, as a therapeutic target in cancer. Following these findings, studies are now testing cannabinoids such as THC and CBD on models of melanoma.
Contents:
Melanoma remains the deadliest form of skin cancer. Hundreds of thousands of people are diagnosed with the disease every year—and numbers are predicted to keep rising. Surgeons are able to remove melanoma when caught early enough, but it quickly spreads to the lymph nodes and beyond when left unchecked. Now, researchers are exploring the role of the endocannabinoid system in cancer, and studies are testing THC and CBD on models of the condition.
What Is Melanoma?
Melanoma is a serious form of skin cancer, of which there are numerous. These conditions are named after the types of skin cells in which they occur. Whereas basal cell carcinoma (BCC) originates in the basal cells of the skin, melanoma forms in melanocytes—the specialized cells that produce the darkening skin pigment melanin in response to UV radiation.
Although less common than other skin cancers, melanoma remains the deadliest. The disease stands as the fifth-most common cancer in the UK, with over 8,000 new cases every year. Among these, 29% of cases occur in patients aged 75 and over. Despite claiming the most lives of any form of skin cancer, the survival rate has doubled over the past 40 years, and now over 87% of patients diagnosed with melanoma survive the disease for the first 10 years or longer.
Although melanoma offers a better prognosis compared to some cancers, the rates of melanoma are projected to increase by 7% by 2035 in the UK alone. With that in mind, what exactly causes melanoma in the first place?
Causes of Melanoma
All cancers stem from a genetic root. Under normal circumstances, damaged or abnormal cells are destroyed and replaced with healthy cells. However, in cases of cancer, these troublesome cells begin to divide, multiply, and sometimes spread throughout the body (a process known as metastasis). Changes to certain genes that control how cells divide and grow underlie cancer. Some of these changes are inherited, whereas others are a direct consequence of environmental factors or lifestyle factors.
When it comes to melanoma, the sun takes most of the blame. But don’t get it twisted—we also need the sun for optimal health. Exposure to the rays emitted from this giant ball of gas allows our skin cells to synthesise vitamin D, a key hormone that helps to quell inflammation and reduce cancer cell growth.
However, the sun’s rays contain ultraviolet (UV) radiation. Excess exposure to UV can damage the DNA in skin cells. This changes the way skin cells function, prompting them to start dividing abnormally—ultimately resulting in skin cancer.
Melanoma Risk Factors
There are several risk factors that increase the chances of a person developing melanoma. These variables include:
| Excess UV exposure | Family history of melanoma | Presence of moles on the skin | Fair skin, freckling, and light hair |
| A history of other skin cancers | Old age | Being male | Compromised immune system |
| Excess UV exposure | Family history of melanoma |
| Presence of moles on the skin | Fair skin, freckling, and light hair |
| A history of other skin cancers | Old age |
| Being male | Compromised immune system |
Symptoms of Melanoma
Melanomas have a similar appearance to normal moles. However, several key visual differences allow physicians to tell them apart. These include:
- They gradually get bigger
- They change shape and color
- They become itchy and sore
- They bleed or develop a crusty appearance
- They are asymmetrical and have a ragged border


Current Treatments for Melanoma
The treatments available for melanoma vary depending on the stage of the disease. Stage 1 and stage 2 melanoma feature cancerous growths that haven’t started to spread. The conventional route during this time involves surgery performed under local anaesthetic to remove the abnormal cells.
Stage 3 melanoma occurs when the cancerous cells spread to nearby lymph nodes. In this case, surgeons perform a lymph node dissection under general anaesthetic. However, this procedure can lead to complications in the lymphatic system that cause fluid to build in the limbs.
A Word on Cannabis and Skin Cancer
So, where does cannabis fit into all of this? Whereas many patients choose to pursue the conventional course of treatment, others decide to look for alternatives. Given the popularity of CBD, you’ll find all sorts of articles online concerning the investigation surrounding CBD and skin cancer. While the internet features scores of anecdotes, the lack of clear-cut science makes this a gamble.
No human trials have explored CBD or cannabis oil for skin cancer. In fact, very few human trials exist testing cannabis against human disease in general; decades of prohibition and the current legal status of cannabis in many countries makes these investigations difficult, if not impossible.
However, these restrictions haven’t stopped researchers from testing cannabinoids on skin cancer cells and animal subjects. These early studies offer insights into what researchers might find when human trials are eventually performed. Below, we’ll take you through these pieces of research. But first, let’s take a brief dive into how cannabinoids work in the body.
The Endocannabinoid System and Cancer
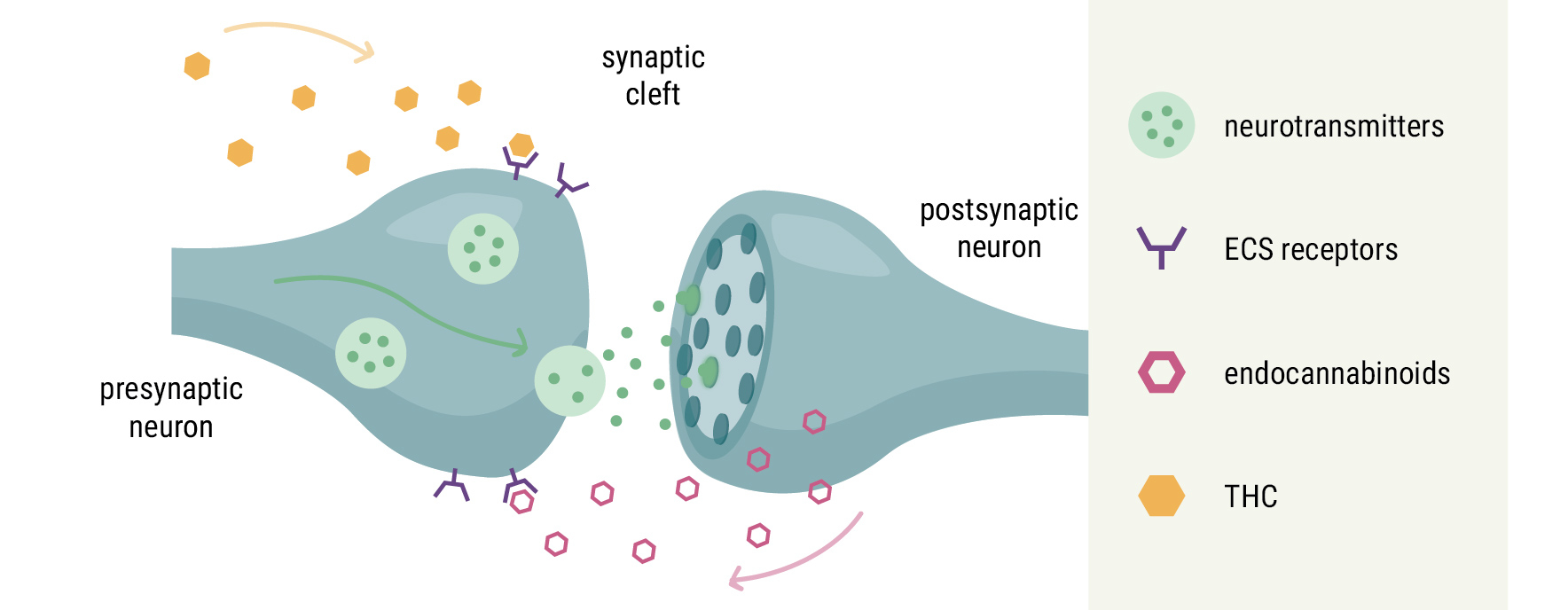
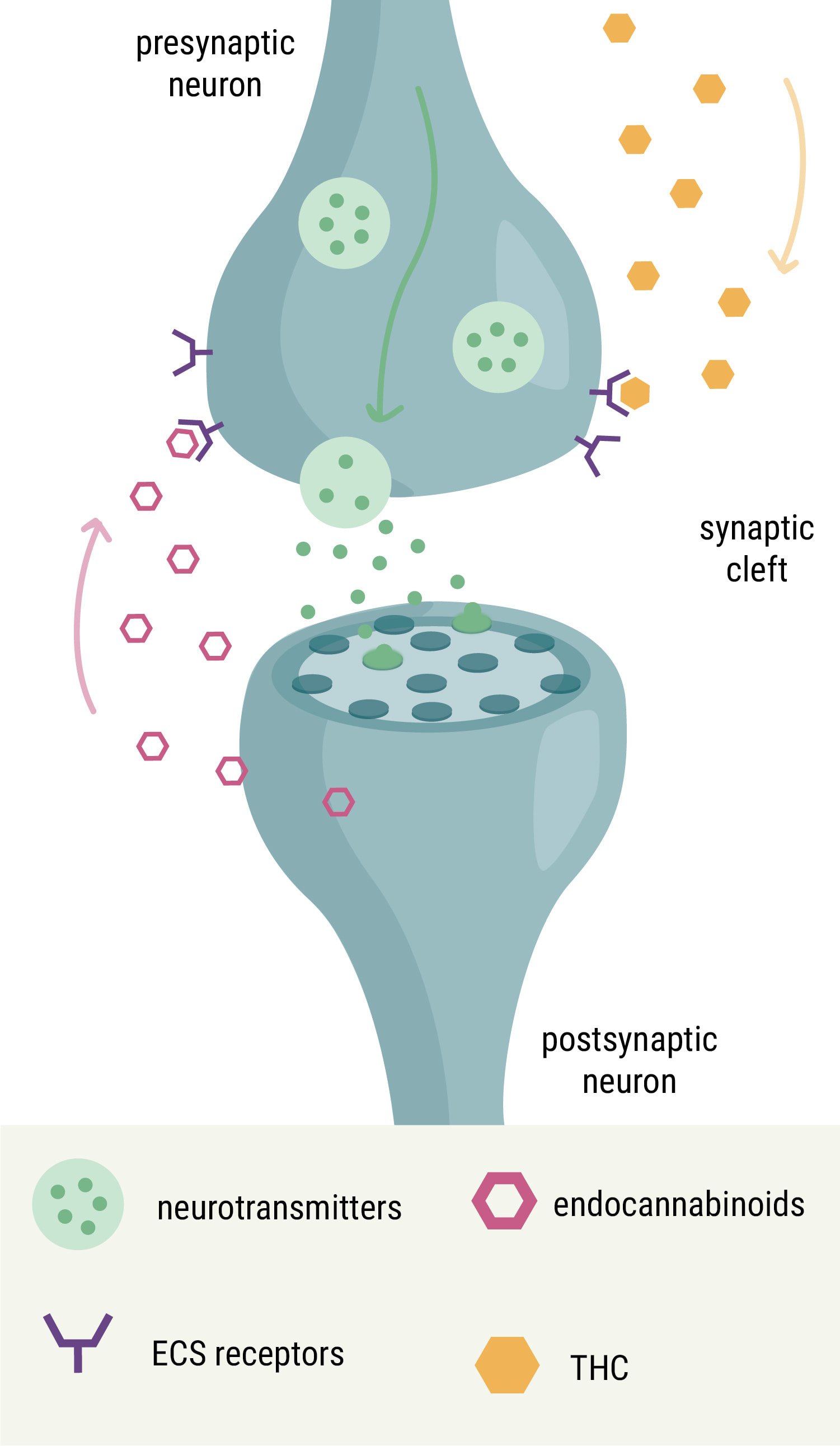
You’ve probably heard of the endocannabinoid system (ECS) by now. This body-wide network, referred to as the universal regulator of the human body, helps to keep all of our other physiological systems in balance (a state known as homeostasis). Researchers discovered the ECS thanks to cannabis. They came across it while investigating how compounds within the plant, namely cannabinoids such as THC, affect the body. Eventually, they discovered a large network of receptors, signalling molecules, and enzymes in many tissues of the body, from the brain and bones to the immune system and digestive system.
But cannabinoids aren’t only present in the cannabis plant; our bodies produce their own version called endocannabinoids (“endo” meaning “within”). ECS enzymes build and break down endocannabinoids on demand, and these signalling molecules bind to ECS receptors to create the necessary changes within a host of different cell types.
At first, scientists discovered two ECS receptors: CB1 and CB2. However, more research has expanded the components into the endocannabinoidome—a massive system that encompasses myriad receptors, enzymes, and signalling molecules.
Because cannabinoids such as THC share a similar structure to our own endocannabinoids, they’re able to bind to the same receptors, in turn influencing the system responsible for keeping other bodily systems in check.
Because ECS components are everywhere, it makes sense that researchers have explored how this system impacts cancer. Thanks to these efforts, scientists discovered that the ECS plays a role in tumorigenesis (the gain of malignant properties of normal cells) and the inhibition of tumour growth. These findings have led some researchers to view ECS receptors as potential therapeutic targets in cancer(s).
Interestingly, the ECS also plays a fundamental role in skin physiology. Here, it helps to control proliferation, growth, differentiation, apoptosis (programmed cell death), and hormone production. The presence of the ECS in the skin, and the potential of the ECS as a therapeutic target in cancer, are driving researchers to explore cannabinoids in models of skin cancer.
What Does the Research Say About Cannabinoids and Melanoma?
The role of cannabinoids in cases of melanoma remains uncertain. Below, we’ll look at the available evidence on THC and CBD in regard to the disease.
THC and Melanoma
You’ve heard of THC. It’s the major psychoactive cannabinoid that underpins the cannabis high. This molecule produces these much-loved effects by binding directly to the CB1 receptor. However, THC also binds to other ECS receptor sites, including CB2.
Researchers are keen to explore how THC impacts melanoma cells, particularly in regard to autophagy—the process by which cells devour themselves when they become damaged. A study published in the Journal of Investigative Dermatology tested THC against melanoma cells, and researchers looked for several outcomes, including the activation of autophagy, loss of cell viability, and the activation of apoptosis.
Further research identified the presence of both CB1 and CB2 on melanoma cells. This prompted scientists to test THC on mice with the disease. They set out to measure any tumour reduction caused by the cannabinoid, and also administered THC to mice with no cannabinoid receptors to compare the difference in outcomes.
CBD and Melanoma
CBD influences the ECS in a much different manner compared to THC. It has a low binding affinity to CB1 and CB2, but it binds to a site known as TRPV1, a suspected third cannabinoid receptor. CBD also interferes with ECS enzymes, namely fatty acid amide hydrolase (FAAH), that break down our endocannabinoids.
Because CBD stands as the second-most abundant cannabinoid in most cultivars, researchers have also conducted studies to see how the molecule affects melanoma. A 2021 paper published in the Journal of Immunoassay and Immunochemistry tested four different concentrations of 99% CBD oil on mouse melanoma cells. During the experiment, they looked for any signs of CBD inhibiting melanoma cell growth.
Another study performed in 2021 tested different CBD formulations on melanoma cells. Researchers administered Charlotte’s Web CBD oil to some cells and purified CBD to others. Throughout the study, they measured effects on cell migration and invasion.
The Rick Simpson Story
Many people became curious about the conversation of cannabis and skin cancer after hearing about Rick Simpson. Upon receiving a basal cell carcinoma diagnosis, this now-famous Canadian decided to apply Rick Simpson oil (RSO)—a high-potency crude cannabis extract. The film Run From the Cure documents his journey. RSO exploded in popularity, and thousands of people have shared their experiences using the preparation online.
The Research on Marijuana and Melanoma Remains Early
Unfortunately, a lack of human studies means it’s far too early to know how cannabis impacts melanoma and skin cancer as a whole. However, early studies focused on the role of the ECS in cancer and the application of cannabinoids in cell and animal models justify further exploration. The use of cannabis for the majority of human diseases remains at this juvenile stage. However, changing legal tides and booming economic interest are set to change this.
If you’re curious about using cannabis for any medical condition, you should always consult your doctor for advice.